Psoriatic arthritis is a chronic inflammatory condition that affects both the skin and joints, leading to pain, stiffness, and swelling that can significantly impact daily life. Early diagnosis and targeted treatment are essential to manage symptoms and prevent joint damage. Discover effective strategies and therapies to help you live well with psoriatic arthritis in the rest of this article.
Table of Comparison
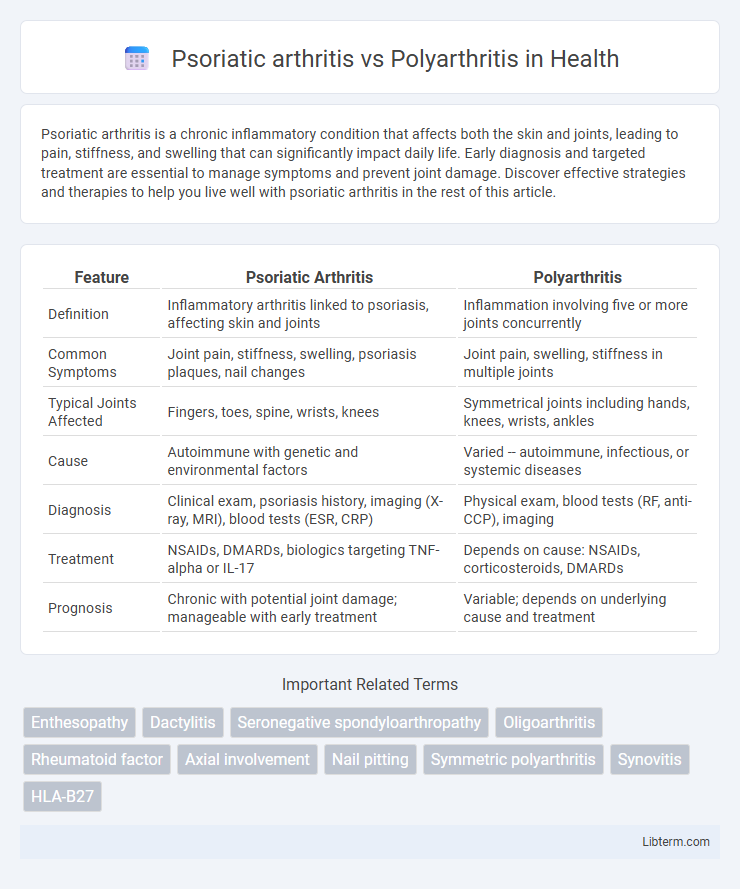
| Feature | Psoriatic Arthritis | Polyarthritis |
|---|---|---|
| Definition | Inflammatory arthritis linked to psoriasis, affecting skin and joints | Inflammation involving five or more joints concurrently |
| Common Symptoms | Joint pain, stiffness, swelling, psoriasis plaques, nail changes | Joint pain, swelling, stiffness in multiple joints |
| Typical Joints Affected | Fingers, toes, spine, wrists, knees | Symmetrical joints including hands, knees, wrists, ankles |
| Cause | Autoimmune with genetic and environmental factors | Varied -- autoimmune, infectious, or systemic diseases |
| Diagnosis | Clinical exam, psoriasis history, imaging (X-ray, MRI), blood tests (ESR, CRP) | Physical exam, blood tests (RF, anti-CCP), imaging |
| Treatment | NSAIDs, DMARDs, biologics targeting TNF-alpha or IL-17 | Depends on cause: NSAIDs, corticosteroids, DMARDs |
| Prognosis | Chronic with potential joint damage; manageable with early treatment | Variable; depends on underlying cause and treatment |
Overview of Psoriatic Arthritis and Polyarthritis
Psoriatic arthritis is a chronic inflammatory arthritis associated with psoriasis, characterized by joint pain, stiffness, and swelling primarily affecting the fingers and toes with distinct skin and nail changes. Polyarthritis involves inflammation of five or more joints simultaneously and can result from various conditions, including rheumatoid arthritis and infections. Both diseases cause joint damage but differ in underlying causes, clinical presentations, and treatment approaches.
Key Differences Between Psoriatic Arthritis and Polyarthritis
Psoriatic arthritis primarily affects individuals with psoriasis, causing joint inflammation, stiffness, and swelling often accompanied by skin symptoms, while polyarthritis refers to inflammation involving five or more joints from various causes including rheumatoid arthritis, lupus, or infections. Diagnosis of psoriatic arthritis relies on clinical features, psoriasis history, and imaging showing joint damage and enthesitis, whereas polyarthritis requires identifying the underlying systemic condition through blood tests and imaging. Treatment for psoriatic arthritis often involves disease-modifying antirheumatic drugs (DMARDs) targeting both skin and joint symptoms, contrasting with polyarthritis management which is tailored to the specific etiology driving joint inflammation.
Causes and Risk Factors
Psoriatic arthritis is an autoimmune condition linked to psoriasis, often triggered by genetic predisposition and environmental factors such as infections or trauma. Polyarthritis, characterized by inflammation in five or more joints, can result from diverse causes including rheumatoid arthritis, infections, or systemic lupus erythematosus. Both conditions share risk factors like family history and immune system dysfunction but differ in their underlying etiology and associated clinical features.
Common Signs and Symptoms
Psoriatic arthritis and polyarthritis both present with joint inflammation characterized by pain, swelling, and stiffness, but psoriatic arthritis often includes skin lesions such as psoriasis plaques and nail changes like pitting or onycholysis. Morning stiffness lasting more than 30 minutes and asymmetric joint involvement are more common in psoriatic arthritis, whereas polyarthritis typically involves symmetric joint swelling, especially in small joints of the hands and feet. Enthesitis, dactylitis (sausage digits), and axial skeletal symptoms frequently accompany psoriatic arthritis but are rare in classic polyarthritis presentations.
Diagnosis and Clinical Assessment
Psoriatic arthritis diagnosis involves clinical examination of joint inflammation combined with skin or nail psoriasis identification and imaging studies such as X-rays or MRI to detect joint damage and enthesitis. Polyarthritis diagnosis requires the evaluation of multiple joint swelling and stiffness through physical examination, laboratory tests including rheumatoid factor (RF) and anti-CCP antibodies, and imaging to differentiate rheumatoid arthritis from other causes. Clinical assessment for both conditions emphasizes symptom duration, joint pattern, presence of systemic features, and response to treatment to guide precise diagnosis and management.
Impact on Joints and Other Body Systems
Psoriatic arthritis primarily affects the joints and surrounding tissues, leading to inflammation, pain, and potential joint deformity, with symptoms often involving the fingers, spine, and sacroiliac joints. Polyarthritis, characterized by inflammation in five or more joints, commonly impacts symmetrical joints like wrists, knees, and ankles, and is frequently associated with systemic involvement such as fatigue, fever, and organ inflammation. Both conditions can cause significant joint damage and functional impairment, but psoriatic arthritis uniquely links to skin psoriasis and enthesitis, while polyarthritis often reflects broader autoimmune conditions like rheumatoid arthritis.
Treatment Options and Management Strategies
Psoriatic arthritis treatment typically includes nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, and biologics targeting TNF-alpha or IL-17 to reduce inflammation and prevent joint damage. Polyarthritis management depends on the underlying cause, with rheumatoid arthritis often treated using a combination of DMARDs, corticosteroids, and biologic agents to control systemic inflammation. Both conditions require a multidisciplinary approach including physical therapy, lifestyle modifications, and regular monitoring to optimize joint function and quality of life.
Prognosis and Long-Term Outlook
Psoriatic arthritis often has a variable prognosis, with some patients experiencing mild symptoms while others develop severe joint damage and disability, often influenced by early diagnosis and treatment adherence. Polyarthritis, characterized by inflammation in five or more joints, typically presents a chronic course, with prognosis depending on the underlying cause, such as rheumatoid arthritis, which may lead to joint deformity if untreated. Long-term management strategies and advances in disease-modifying therapies significantly improve functional outcomes and quality of life in both conditions.
Living with Psoriatic Arthritis vs Polyarthritis
Living with psoriatic arthritis often involves managing joint pain, stiffness, and skin symptoms, requiring tailored treatment plans including biologics and lifestyle adjustments to reduce flare-ups. Polyarthritis, characterized by inflammation in five or more joints, demands comprehensive approaches focusing on symptom control, physical therapy, and sometimes disease-modifying antirheumatic drugs (DMARDs) to prevent joint damage. Both conditions necessitate regular medical monitoring and personalized strategies to maintain mobility and quality of life.
Frequently Asked Questions
Psoriatic arthritis is an inflammatory arthritis associated with psoriasis, often affecting joints asymmetrically and involving entheses, while polyarthritis refers to inflammation in five or more joints, commonly symmetric, seen in conditions like rheumatoid arthritis. Frequently asked questions highlight differences in symptoms, such as skin psoriasis presence in psoriatic arthritis versus widespread joint swelling in polyarthritis, diagnostic markers like elevated ESR or CRP, and treatment options including biologics targeting specific immune pathways. Understanding the distinct clinical features and laboratory findings assists in accurate diagnosis and personalized management plans for both conditions.
Psoriatic arthritis Infographic
 libterm.com
libterm.com