Neutrophilic lymphocytic infiltration refers to the presence of both neutrophils and lymphocytes in tissue, indicating an active immune response often related to infection or inflammation. This mixed cell population can suggest various underlying conditions, from acute bacterial infections to chronic inflammatory diseases. Explore the rest of the article to understand how this cellular pattern impacts diagnosis and treatment options for your health.
Table of Comparison
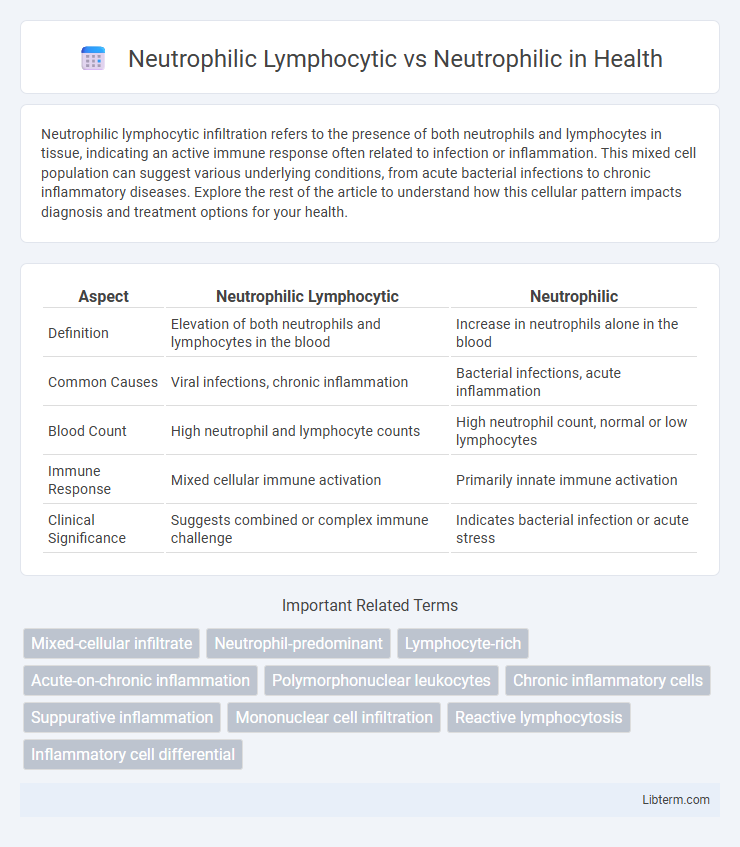
| Aspect | Neutrophilic Lymphocytic | Neutrophilic |
|---|---|---|
| Definition | Elevation of both neutrophils and lymphocytes in the blood | Increase in neutrophils alone in the blood |
| Common Causes | Viral infections, chronic inflammation | Bacterial infections, acute inflammation |
| Blood Count | High neutrophil and lymphocyte counts | High neutrophil count, normal or low lymphocytes |
| Immune Response | Mixed cellular immune activation | Primarily innate immune activation |
| Clinical Significance | Suggests combined or complex immune challenge | Indicates bacterial infection or acute stress |
Understanding Neutrophilic Lymphocytic Infiltration
Neutrophilic lymphocytic infiltration involves the simultaneous presence of neutrophils and lymphocytes in tissue, indicating a complex immune response often seen in chronic inflammation or infection. Unlike pure neutrophilic infiltration, which primarily signals acute bacterial infection, the combined infiltration suggests both innate and adaptive immune activation. Recognizing the balance between these cells is crucial for accurate diagnosis and tailored therapeutic strategies in inflammatory and autoimmune diseases.
What is Pure Neutrophilic Infiltration?
Pure neutrophilic infiltration refers to the presence of neutrophils exclusively or predominantly within a tissue, indicating an acute inflammatory response typically caused by bacterial infections or tissue injury. In contrast, neutrophilic lymphocytic infiltration involves a mixed population of neutrophils and lymphocytes, reflecting a broader immune response that may be associated with viral infections or chronic inflammation. Identifying pure neutrophilic infiltration aids in diagnosing acute bacterial conditions and guides appropriate antibiotic therapy.
Key Differences Between Neutrophilic Lymphocytic and Neutrophilic Patterns
Neutrophilic lymphocytic patterns feature a mixed infiltration of neutrophils and lymphocytes, indicating both acute and chronic inflammatory responses, whereas neutrophilic patterns predominantly consist of neutrophil infiltration associated mainly with acute inflammation. Neutrophilic lymphocytic inflammation often occurs in autoimmune diseases or chronic infections, while pure neutrophilic patterns are typical of bacterial infections or acute tissue injury. The cellular composition in these patterns influences diagnostic and therapeutic approaches, guiding targeted treatment for inflammation type and underlying cause.
Pathophysiology of Neutrophilic Lymphocytic Conditions
Neutrophilic lymphocytic conditions involve a complex immune response characterized by simultaneous activation and infiltration of neutrophils and lymphocytes, indicating both innate and adaptive immune system engagement. The pathophysiology includes cytokine-mediated signaling pathways such as interleukin-8 (IL-8) promoting neutrophil chemotaxis, alongside T-cell activation driving lymphocytic infiltration, contributing to sustained inflammation and tissue damage. This dual-cell involvement distinguishes neutrophilic lymphocytic conditions from purely neutrophilic disorders, which primarily feature acute innate immune responses without significant lymphocyte participation.
Common Diseases with Neutrophilic Lymphocytic Infiltrates
Neutrophilic lymphocytic infiltrates commonly occur in autoimmune diseases such as rheumatoid arthritis and lupus erythematosus, where both neutrophils and lymphocytes participate in tissue inflammation. Infectious diseases like tuberculosis and certain viral infections also demonstrate mixed neutrophilic and lymphocytic infiltrates, reflecting a complex immune response. In contrast, purely neutrophilic infiltrates are predominantly seen in acute bacterial infections such as abscesses and acute appendicitis.
Clinical Significance of Pure Neutrophilic Responses
Pure neutrophilic responses are clinically significant as they typically indicate acute bacterial infections, inflammation, or tissue damage, reflecting the body's immediate defense mechanism against pathogens. Unlike neutrophilic lymphocytic responses, which suggest a combined immune activation involving both neutrophils and lymphocytes, a pure neutrophilic profile helps differentiate conditions such as bacterial sepsis or acute appendicitis from viral infections or chronic inflammatory diseases. Monitoring neutrophil counts and activity provides critical insights for diagnosis, prognosis, and treatment efficacy in various medical conditions.
Histopathological Features: Neutrophilic Lymphocytic vs Neutrophilic
Neutrophilic lymphocytic infiltrates display a mixed composition of neutrophils and lymphocytes within tissue sections, often indicating a combined acute and chronic inflammatory response. In contrast, purely neutrophilic infiltrates are predominantly composed of neutrophils, reflecting an acute inflammatory process with abundant polymorphonuclear leukocytes. Histopathologically, neutrophilic lymphocytic infiltration may present with perivascular lymphocytic aggregates alongside neutrophilic exocytosis, whereas neutrophilic infiltration is characterized by dense clusters of neutrophils, often accompanied by tissue necrosis or abscess formation.
Diagnostic Strategies for Differentiating These Patterns
Neutrophilic lymphocytic and neutrophilic patterns require distinct diagnostic strategies centered on comprehensive blood count analysis and differential leukocyte profiling. Advanced flow cytometry and immunohistochemical staining help distinguish the predominance of neutrophils versus mixed neutrophilic and lymphocytic infiltration in tissue samples. Molecular testing for cytokine profiles and genetic markers further refines diagnosis by identifying underlying inflammatory or infectious etiologies associated with each cellular pattern.
Treatment Implications and Prognosis
Neutrophilic lymphocytic inflammation often indicates a combined immune response requiring tailored treatment strategies that address both neutrophil-driven and lymphocyte-mediated pathways, potentially involving corticosteroids and immunomodulatory agents. In contrast, purely neutrophilic inflammation typically responds well to antibiotics targeting bacterial infections, with a generally favorable prognosis if treated promptly. Understanding the dominant cellular profile improves prognosis accuracy and guides therapeutic decisions in inflammatory diseases.
Future Perspectives in Research and Clinical Practice
Future perspectives in research and clinical practice of neutrophilic lymphocytic versus neutrophilic inflammation emphasize advanced biomarker discovery and precision medicine approaches. Emerging studies focus on the differential cytokine profiles and immune cell interactions to develop targeted therapies that improve patient outcomes in chronic inflammatory diseases. Integration of multi-omics data and artificial intelligence in clinical diagnostics promises to refine phenotypic classifications and guide personalized treatment strategies.
Neutrophilic Lymphocytic Infographic
 libterm.com
libterm.com