Adenoidectomy is a surgical procedure that removes the adenoids, which are lymphatic tissues located behind the nasal cavity that can cause breathing difficulties, recurring infections, or sleep apnea when enlarged. This operation is commonly performed on children to improve nasal airflow and reduce the frequency of ear and sinus infections. Discover how adenoidectomy could benefit your child's health and what to expect during recovery in the rest of this article.
Table of Comparison
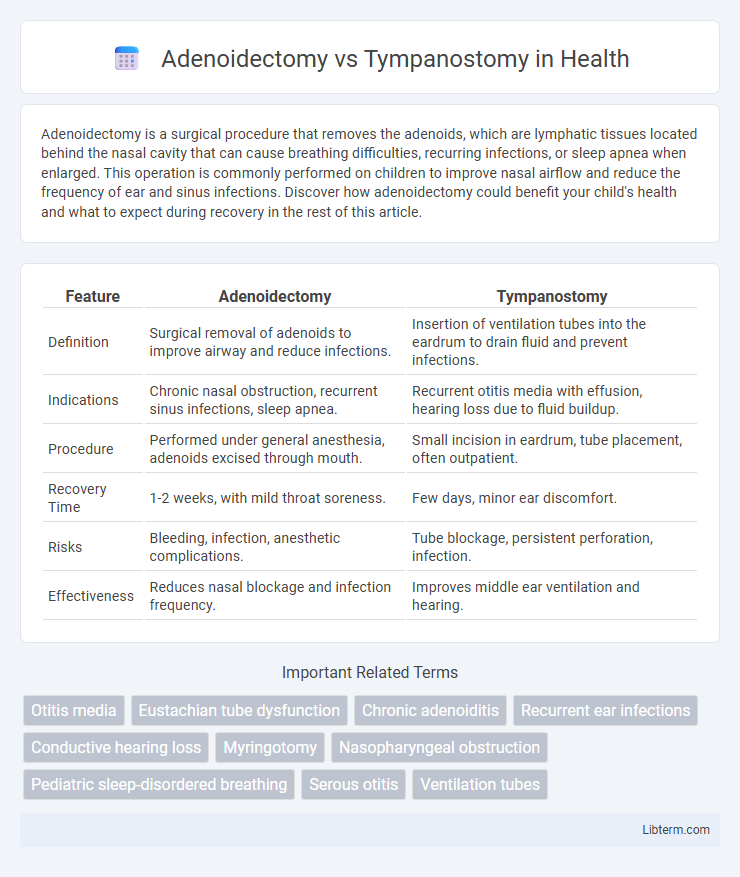
| Feature | Adenoidectomy | Tympanostomy |
|---|---|---|
| Definition | Surgical removal of adenoids to improve airway and reduce infections. | Insertion of ventilation tubes into the eardrum to drain fluid and prevent infections. |
| Indications | Chronic nasal obstruction, recurrent sinus infections, sleep apnea. | Recurrent otitis media with effusion, hearing loss due to fluid buildup. |
| Procedure | Performed under general anesthesia, adenoids excised through mouth. | Small incision in eardrum, tube placement, often outpatient. |
| Recovery Time | 1-2 weeks, with mild throat soreness. | Few days, minor ear discomfort. |
| Risks | Bleeding, infection, anesthetic complications. | Tube blockage, persistent perforation, infection. |
| Effectiveness | Reduces nasal blockage and infection frequency. | Improves middle ear ventilation and hearing. |
Overview of Adenoidectomy and Tympanostomy
Adenoidectomy involves the surgical removal of the adenoids to treat chronic infections or breathing difficulties, often improving nasal airflow and reducing ear infections. Tympanostomy, commonly known as ear tube surgery, entails placing small tubes in the eardrum to ventilate the middle ear and prevent fluid accumulation, primarily addressing recurrent otitis media with effusion. Both procedures target ENT-related complications but serve distinct purposes based on the underlying condition--adenoid enlargement or middle ear ventilation issues.
Indications for Each Procedure
Adenoidectomy is primarily indicated for recurrent or chronic adenoid hypertrophy causing nasal obstruction, obstructive sleep apnea, or recurrent otitis media with effusion. Tympanostomy tubes are indicated for persistent middle ear effusion lasting more than three months, recurrent acute otitis media with otitis media with effusion, or hearing loss related to effusion. Both procedures address Eustachian tube dysfunction, but adenoidectomy targets obstruction from adenoidal tissue, while tympanostomy facilitates middle ear ventilation.
Surgical Techniques: How Are They Performed?
Adenoidectomy involves the surgical removal of the adenoids using curettes or microdebriders through the mouth, typically under general anesthesia, to clear airway obstruction and reduce infections. Tympanostomy, also known as ear tube surgery, requires creating a small incision in the eardrum to insert ventilation tubes that equalize ear pressure and drain fluid, performed under microscopic guidance. Both procedures are minimally invasive, aiming to improve respiratory function and ear health in pediatric patients with recurrent infections or ventilation issues.
Patient Age and Suitability
Adenoidectomy is most suitable for children aged 3 to 7 years with recurrent adenoid infections or obstructive sleep apnea, while tympanostomy is generally indicated for younger children, often under 3 years, experiencing chronic otitis media with effusion or frequent ear infections. Patient age significantly influences the choice, as adenoidectomy addresses airway obstruction and infection in older children, whereas tympanostomy focuses on middle ear ventilation in infants and toddlers. Clinical guidelines recommend considering developmental milestones and immune system maturity when determining the appropriate procedure for pediatric otolaryngology patients.
Benefits of Adenoidectomy
Adenoidectomy effectively reduces recurrent ear infections and improves nasal airway obstruction by removing inflamed adenoid tissue located near the Eustachian tubes. This procedure enhances Eustachian tube function, thereby decreasing middle ear fluid buildup and promoting better hearing compared to tympanostomy alone. Patients experience fewer respiratory infections and reduced dependency on tubes, leading to improved overall ear and upper respiratory health.
Benefits of Tympanostomy
Tympanostomy offers targeted relief by ventilating the middle ear and preventing fluid accumulation, significantly reducing the frequency of ear infections and improving hearing in children with recurrent otitis media. This minimally invasive procedure promotes rapid recovery with fewer complications compared to adenoidectomy, which primarily addresses nasal obstruction and chronic adenoiditis. Tympanostomy's benefits include improved middle ear aeration, decreased need for systemic antibiotics, and enhanced quality of life by reducing otologic symptoms.
Risks and Complications Compared
Adenoidectomy carries risks such as bleeding, infection, and potential velopharyngeal insufficiency, while tympanostomy involves risks including persistent ear drainage, infection, and possible tympanic membrane perforation. Complications from adenoidectomy may lead to nasal regurgitation or voice changes, whereas tympanostomy tube placement can occasionally cause scarring or chronic otitis media. Both procedures require careful evaluation of patient history and close postoperative monitoring to mitigate adverse outcomes.
Recovery and Aftercare
Recovery after adenoidectomy typically involves mild throat pain and nasal congestion, with most patients resuming normal activities within 7 to 10 days. Tympanostomy tube insertion requires careful ear care to prevent infection, with ear drainage and temporary hearing changes being common but usually resolving within a few weeks. Both procedures necessitate follow-up appointments to monitor healing and address potential complications such as infection or tube blockage.
Long-Term Outcomes and Recurrence Rates
Adenoidectomy typically shows superior long-term outcomes in reducing recurrent otitis media compared to tympanostomy alone, as it addresses underlying nasopharyngeal obstruction and bacterial reservoirs. Tympanostomy tubes provide immediate symptom relief by ventilating the middle ear and preventing fluid accumulation but may have higher recurrence rates once tubes extrude. Combining adenoidectomy with tympanostomy is often recommended for children with persistent middle ear infections to optimize sustained disease control and minimize recurrence.
Choosing the Right Procedure for Individual Patients
Selecting the appropriate procedure between adenoidectomy and tympanostomy depends on the patient's specific symptoms and underlying conditions, such as chronic ear infections or obstructive sleep apnea. Adenoidectomy is typically favored for patients with enlarged adenoids causing nasal obstruction or recurrent infections, while tympanostomy is preferred for those experiencing persistent middle ear fluid or hearing loss due to Eustachian tube dysfunction. Comprehensive evaluation by an otolaryngologist, including medical history and audiological assessments, ensures tailored treatment that minimizes complications and maximizes patient outcomes.
Adenoidectomy Infographic
 libterm.com
libterm.com