Neutropenia and pancytopenia are hematological conditions characterized by a significant reduction in blood cell counts, affecting your immune system and overall health. Neutropenia specifically involves a low neutrophil count, increasing infection risk, while pancytopenia results in the decrease of all blood cells, causing fatigue, bruising, and bleeding. Explore the detailed distinctions, causes, and treatment options in the rest of this article to better understand these critical disorders.
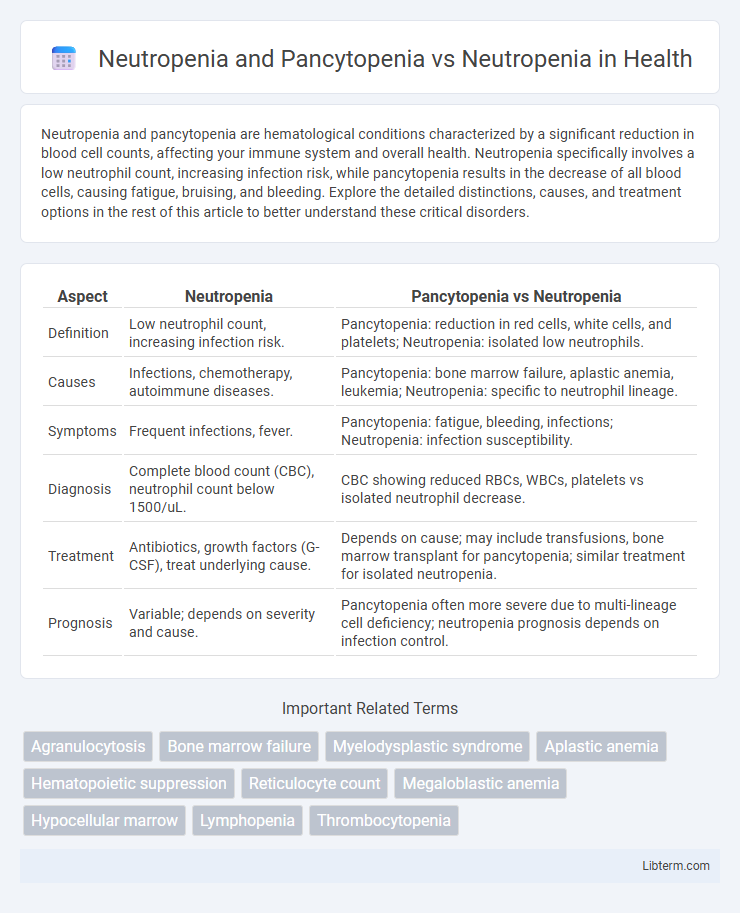
Table of Comparison
| Aspect | Neutropenia | Pancytopenia vs Neutropenia |
|---|---|---|
| Definition | Low neutrophil count, increasing infection risk. | Pancytopenia: reduction in red cells, white cells, and platelets; Neutropenia: isolated low neutrophils. |
| Causes | Infections, chemotherapy, autoimmune diseases. | Pancytopenia: bone marrow failure, aplastic anemia, leukemia; Neutropenia: specific to neutrophil lineage. |
| Symptoms | Frequent infections, fever. | Pancytopenia: fatigue, bleeding, infections; Neutropenia: infection susceptibility. |
| Diagnosis | Complete blood count (CBC), neutrophil count below 1500/uL. | CBC showing reduced RBCs, WBCs, platelets vs isolated neutrophil decrease. |
| Treatment | Antibiotics, growth factors (G-CSF), treat underlying cause. | Depends on cause; may include transfusions, bone marrow transplant for pancytopenia; similar treatment for isolated neutropenia. |
| Prognosis | Variable; depends on severity and cause. | Pancytopenia often more severe due to multi-lineage cell deficiency; neutropenia prognosis depends on infection control. |
Understanding Neutropenia: Definition and Causes
Neutropenia is characterized by an abnormally low count of neutrophils, a type of white blood cell essential for fighting bacterial infections. Causes of neutropenia include bone marrow disorders, autoimmune diseases, certain medications, infections, and chemotherapy. Pancytopenia involves the reduction of all three blood cell types--red cells, white cells, and platelets--but neutropenia specifically targets neutrophil deficiency.
What Is Pancytopenia? Key Differences from Neutropenia
Pancytopenia is a medical condition characterized by the simultaneous reduction of all three blood cell types: red blood cells, white blood cells (including neutrophils), and platelets. In contrast, neutropenia specifically refers to a decrease in the neutrophil count, a subtype of white blood cells critical for fighting infections. The key difference lies in pancytopenia's broader impact on multiple blood cell lines, leading to symptoms like anemia, increased infection risk, and bleeding tendencies, whereas neutropenia primarily increases susceptibility to infections due to low neutrophil levels.
Overlapping and Distinct Symptoms: Neutropenia versus Pancytopenia
Neutropenia primarily involves a decreased neutrophil count, leading to increased susceptibility to bacterial infections, while pancytopenia affects all three blood cell lines--red cells, white cells, and platelets--causing symptoms like anemia, bleeding tendencies, and heightened infection risk. Overlapping symptoms include frequent infections and general fatigue due to compromised immune response. Distinctly, pancytopenia presents with additional manifestations such as petechiae, bruising, and pallor, reflecting multi-lineage bone marrow suppression unlike isolated neutropenia.
Pathophysiology: Neutrophil vs. Multilineage Cell Reduction
Neutropenia primarily involves a reduction in neutrophil count due to impaired production, increased destruction, or altered distribution, impacting the body's ability to fight bacterial infections. Pancytopenia encompasses a broader multilineage cell reduction, including neutrophils, erythrocytes, and platelets, resulting from bone marrow failure or infiltration, leading to combined immunodeficiency, anemia, and bleeding risks. The pathophysiology of pancytopenia reflects a more extensive marrow suppression or damage compared to the isolated neutrophil lineage defect seen in neutropenia.
Diagnostic Criteria: Blood Work and Laboratory Findings
Neutropenia is characterized by an absolute neutrophil count (ANC) below 1500 cells/uL, with severe cases presenting ANC under 500 cells/uL, typically identified through a complete blood count (CBC) with differential. Pancytopenia involves a reduction in all three blood cell lines--neutrophils, erythrocytes, and platelets--demonstrated by low ANC, hemoglobin, and platelet counts on CBC and confirmed through bone marrow biopsy revealing hypoplasia or aplasia. Laboratory findings in pancytopenia often include additional markers such as elevated serum ferritin and lactate dehydrogenase (LDH), which help differentiate it from isolated neutropenia, emphasizing the importance of comprehensive hematological evaluation.
Common Underlying Conditions: From Infections to Malignancies
Neutropenia and pancytopenia often share underlying conditions such as severe bacterial or viral infections that suppress bone marrow function, while isolated neutropenia commonly arises from viral infections or autoimmune disorders. Malignancies like leukemia and myelodysplastic syndromes frequently present with pancytopenia due to marrow infiltration or fibrosis, contrasting with neutropenia which may occur independently in hematologic cancers or as a side effect of chemotherapy. Identifying specific causes through bone marrow biopsy and blood tests is crucial for differentiating these conditions and guiding appropriate treatment strategies.
Clinical Implications: Infection Risk and Complications
Neutropenia significantly increases infection risk due to reduced neutrophil count, impairing the body's ability to fight bacterial and fungal pathogens. Pancytopenia, involving simultaneous reductions in neutrophils, red blood cells, and platelets, presents compounded clinical implications including severe infection risk, anemia-related fatigue, and bleeding complications. The management of pancytopenia requires vigilant monitoring for infections alongside addressing multifactorial hematologic deficits to reduce morbidity and mortality.
Treatment Approaches: Neutropenia versus Pancytopenia Management
Treatment approaches for neutropenia primarily focus on addressing the underlying cause, administering granulocyte colony-stimulating factor (G-CSF) to boost neutrophil production, and preventing infections with antibiotics or antifungals. Pancytopenia management requires a broader strategy, including bone marrow biopsy to diagnose conditions such as aplastic anemia or hematologic malignancies, supportive care like transfusions for anemia and thrombocytopenia, and potential use of immunosuppressive therapy or hematopoietic stem cell transplantation. Both conditions emphasize infection prevention but pancytopenia demands a multidisciplinary approach targeting all deficient blood cell lines for effective management.
Prognosis and Long-Term Outcomes
Neutropenia combined with pancytopenia typically indicates a more severe underlying bone marrow dysfunction, leading to a poorer prognosis and heightened risk of infections and bleeding complications compared to isolated neutropenia. Long-term outcomes for patients with pancytopenia depend heavily on the cause, with conditions like aplastic anemia or myelodysplastic syndromes requiring intensive treatment and close monitoring. Isolated neutropenia generally has a better prognosis, especially if caused by transient factors or managed appropriately to prevent severe infections.
Key Points: Distinguishing and Managing These Hematologic Disorders
Neutropenia involves a decreased neutrophil count, increasing infection risk, whereas pancytopenia presents with reduced levels of all three blood cell lines--red cells, white cells, and platelets--indicating more extensive bone marrow dysfunction. Diagnosing pancytopenia requires comprehensive evaluation of bone marrow biopsy and peripheral blood smear, while isolated neutropenia may be managed with granulocyte colony-stimulating factor (G-CSF) and infection prophylaxis. Differentiating these conditions is critical for targeted treatment, as pancytopenia often necessitates addressing underlying causes like aplastic anemia or malignancy, whereas neutropenia management focuses on infection prevention and immune modulation.
Neutropenia and Pancytopenia Infographic
 libterm.com
libterm.com