Cholestasis is a condition characterized by the impaired flow of bile from the liver, leading to the accumulation of bile acids in the bloodstream and causing symptoms such as itching, jaundice, and fatigue. Understanding the causes, symptoms, and treatments of cholestasis is essential for effective management and prevention of liver damage. Explore the article to learn how you can recognize and address cholestasis for better liver health.
Table of Comparison
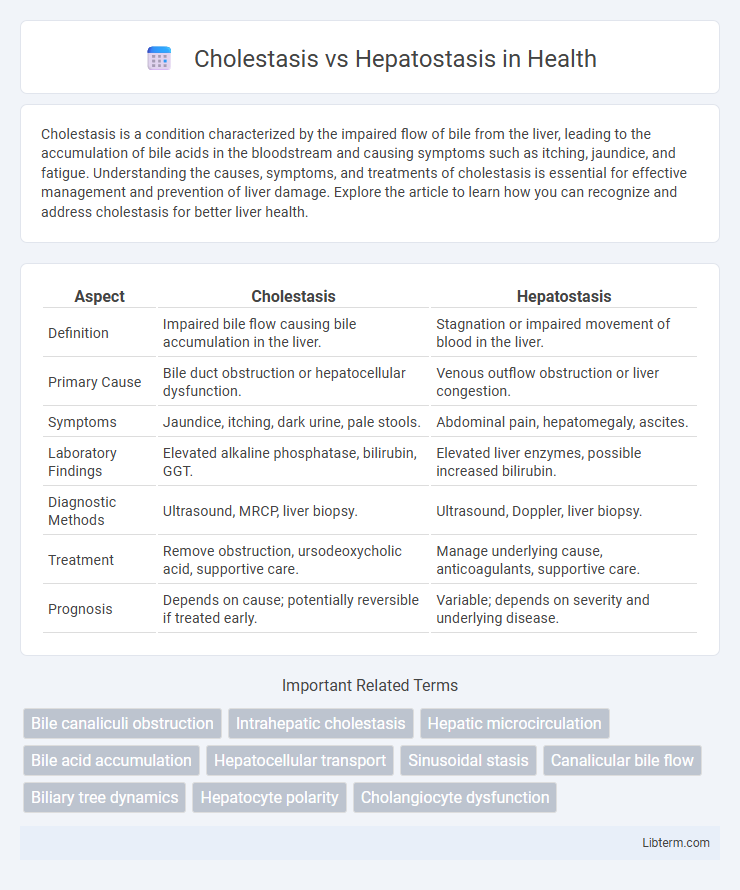
| Aspect | Cholestasis | Hepatostasis |
|---|---|---|
| Definition | Impaired bile flow causing bile accumulation in the liver. | Stagnation or impaired movement of blood in the liver. |
| Primary Cause | Bile duct obstruction or hepatocellular dysfunction. | Venous outflow obstruction or liver congestion. |
| Symptoms | Jaundice, itching, dark urine, pale stools. | Abdominal pain, hepatomegaly, ascites. |
| Laboratory Findings | Elevated alkaline phosphatase, bilirubin, GGT. | Elevated liver enzymes, possible increased bilirubin. |
| Diagnostic Methods | Ultrasound, MRCP, liver biopsy. | Ultrasound, Doppler, liver biopsy. |
| Treatment | Remove obstruction, ursodeoxycholic acid, supportive care. | Manage underlying cause, anticoagulants, supportive care. |
| Prognosis | Depends on cause; potentially reversible if treated early. | Variable; depends on severity and underlying disease. |
Introduction to Cholestasis and Hepatostasis
Cholestasis is a medical condition characterized by the impairment of bile flow from the liver to the duodenum, causing the accumulation of bile acids in the liver and bloodstream, which can lead to jaundice and pruritus. Hepatostasis, less commonly discussed, refers to the stagnation or impaired function of hepatocytes, often resulting in disrupted liver metabolism without necessarily affecting bile flow. Understanding the distinction between cholestasis as a bile flow disorder and hepatostasis as hepatocyte dysfunction is crucial for accurate diagnosis and targeted therapeutic strategies in hepatic diseases.
Defining Cholestasis: Causes and Mechanisms
Cholestasis is a condition characterized by impaired bile flow due to obstruction or defects in bile secretion, often caused by liver diseases like hepatitis, gallstones, or bile duct strictures. This disruption leads to accumulation of bile acids and bilirubin in the liver and bloodstream, causing jaundice and pruritus. Understanding the molecular mechanisms involves impaired transporter proteins such as the bile salt export pump (BSEP) and multidrug resistance-associated protein 2 (MRP2), resulting in hepatocellular damage.
Hepatostasis Explained: Pathophysiology and Triggers
Hepatostasis involves the impaired flow of bile within liver cells or intrahepatic bile ducts, primarily caused by hepatocellular dysfunction or inflammation, leading to bile retention and subsequent liver damage. Key triggers include viral hepatitis, drug-induced liver injury, and autoimmune diseases, which disrupt bile secretion and liver metabolism at the cellular level. Understanding hepatostasis pathophysiology highlights the importance of intracellular bile transport mechanisms and immune responses in maintaining hepatic health.
Key Differences Between Cholestasis and Hepatostasis
Cholestasis involves impaired bile flow resulting in bile accumulation within the liver, causing jaundice, pruritus, and elevated serum bile acids and alkaline phosphatase levels. Hepatostasis refers to the stagnation of blood flow within the liver sinusoids leading to congestion and hepatocyte damage without directly affecting bile secretion. The key difference lies in cholestasis primarily disrupting bile excretion, whereas hepatostasis pertains to vascular abnormalities causing hepatic blood flow impairment.
Clinical Signs and Symptoms of Cholestasis
Cholestasis manifests clinically with jaundice, pruritus, dark urine, pale stools, and fatigue due to impaired bile flow and accumulation of bile components. Patients may exhibit hepatomegaly and right upper quadrant discomfort, reflecting underlying liver dysfunction. In contrast, hepatostasis, involving temporary liver blood flow stasis, typically lacks these cholestatic symptoms and presents with less specific signs related to congestion rather than bile retention.
Clinical Manifestations of Hepatostasis
Hepatostasis typically presents with jaundice, pruritus, and dark urine due to impaired bile flow within the liver, leading to the accumulation of bile acids and bilirubin. Patients may also experience hepatomegaly and right upper quadrant discomfort, reflecting liver inflammation and congestion. Laboratory findings usually include elevated serum alkaline phosphatase, gamma-glutamyl transferase, and conjugated hyperbilirubinemia, distinguishing hepatostasis from cholestasis caused by extrahepatic obstruction.
Diagnostic Approaches: Cholestasis vs Hepatostasis
Diagnostic approaches for cholestasis prioritize biochemical markers such as elevated alkaline phosphatase and gamma-glutamyl transferase levels, alongside imaging techniques like ultrasound or MRCP to identify bile duct obstruction. In contrast, hepatostasis diagnosis focuses on liver function tests displaying impaired synthetic capacity, including decreased albumin and prolonged prothrombin time, supplemented by liver biopsy to assess hepatocyte viability and fibrosis. Differentiating these conditions relies on combining serological profiles with targeted radiologic and histopathological evaluation to determine the underlying hepatic functional impairment versus biliary flow disruption.
Common Complications and Associated Risks
Cholestasis commonly leads to complications such as pruritus, fat malabsorption, and fat-soluble vitamin deficiencies due to impaired bile flow, increasing the risk of osteoporosis and coagulopathy. Hepatostasis primarily results in hepatic congestion and liver dysfunction, which can cause portal hypertension, ascites, and hepatic encephalopathy. Both conditions significantly elevate the risk of progressive liver damage, fibrosis, and potential cirrhosis if untreated.
Current Treatment Strategies for Both Conditions
Current treatment strategies for cholestasis primarily include the use of ursodeoxycholic acid (UDCA) to improve bile flow and reduce liver damage, alongside symptom management with cholestyramine for pruritus and vitamin supplementation to address malabsorption. Hepatostasis treatment focuses on supportive care to maintain liver function, with management of underlying causes such as infections, toxins, or metabolic disorders, and in severe cases, liver transplantation may be necessary. Emerging therapies for both conditions emphasize targeting molecular pathways involved in bile acid regulation and liver regeneration to enhance therapeutic outcomes.
Prognosis and Long-Term Management Considerations
Cholestasis prognosis varies depending on the underlying cause, with potential progression to liver fibrosis or cirrhosis if untreated, requiring therapies aimed at reducing bile duct obstruction and managing symptoms like pruritus. Hepatostasis, characterized by impaired liver function without bile flow obstruction, often necessitates addressing hepatic inflammation or damage through antiviral or immunosuppressive treatments, impacting long-term liver function preservation. Long-term management strategies for both conditions emphasize regular monitoring of liver enzymes, imaging studies, and lifestyle modifications to prevent disease progression and improve overall liver health.
Cholestasis Infographic
 libterm.com
libterm.com