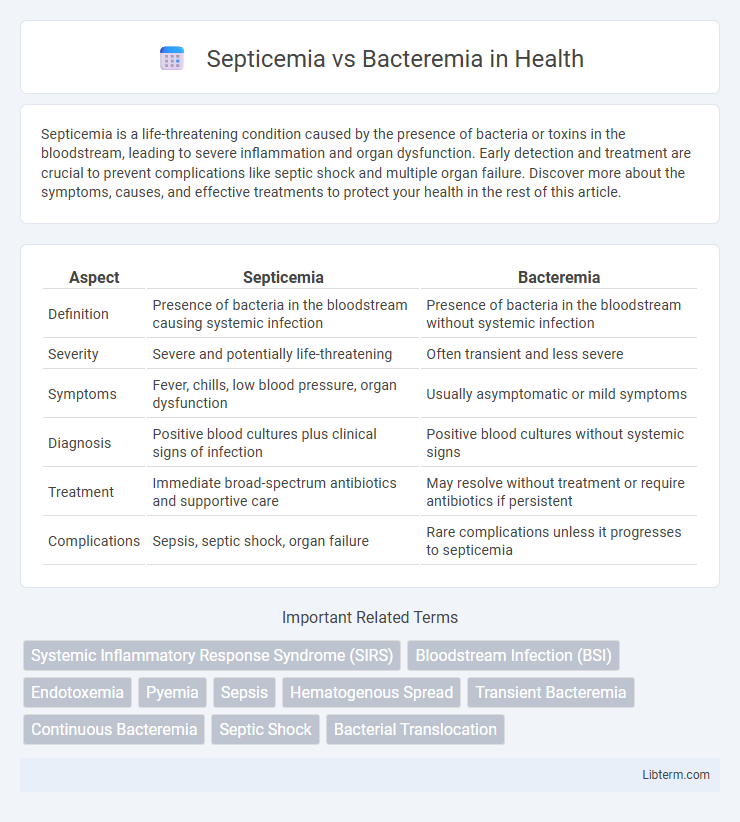
Septicemia is a life-threatening condition caused by the presence of bacteria or toxins in the bloodstream, leading to severe inflammation and organ dysfunction. Early detection and treatment are crucial to prevent complications like septic shock and multiple organ failure. Discover more about the symptoms, causes, and effective treatments to protect your health in the rest of this article.
Table of Comparison
| Aspect | Septicemia | Bacteremia |
|---|---|---|
| Definition | Presence of bacteria in the bloodstream causing systemic infection | Presence of bacteria in the bloodstream without systemic infection |
| Severity | Severe and potentially life-threatening | Often transient and less severe |
| Symptoms | Fever, chills, low blood pressure, organ dysfunction | Usually asymptomatic or mild symptoms |
| Diagnosis | Positive blood cultures plus clinical signs of infection | Positive blood cultures without systemic signs |
| Treatment | Immediate broad-spectrum antibiotics and supportive care | May resolve without treatment or require antibiotics if persistent |
| Complications | Sepsis, septic shock, organ failure | Rare complications unless it progresses to septicemia |
Introduction to Septicemia and Bacteremia
Septicemia is a serious bloodstream infection characterized by the presence and rapid multiplication of pathogenic bacteria leading to systemic inflammatory response and potential organ failure. Bacteremia refers to the presence of bacteria in the bloodstream without systemic symptoms, often transient and cleared by the immune system. Understanding the distinction between bacteremia and septicemia is crucial for timely diagnosis and treatment to prevent progression to severe sepsis or septic shock.
Definitions: Septicemia vs Bacteremia
Septicemia refers to a serious bloodstream infection causing systemic inflammation and symptoms of sepsis, often resulting from the proliferation of pathogens in the blood. Bacteremia describes the presence of bacteria in the bloodstream, which may be transient or persistent but does not always cause systemic illness. Distinguishing septicemia from bacteremia involves recognizing the clinical impact, as septicemia includes signs of infection-induced organ dysfunction, whereas bacteremia can be asymptomatic or less severe.
Causes and Risk Factors
Septicemia is primarily caused by a bacterial infection entering the bloodstream, often originating from sources like pneumonia, urinary tract infections, or surgical wounds, posing significant risks such as weakened immunity, chronic illnesses, or invasive medical procedures. Bacteremia involves the presence of bacteria in the blood, frequently resulting from dental procedures, intravenous drug use, or infections elsewhere in the body, with risk factors including immunosuppression, heart valve disease, and recent surgery. Both conditions require prompt medical attention due to the potential for severe systemic inflammation and organ failure.
Key Differences Between Septicemia and Bacteremia
Septicemia is a severe bloodstream infection causing systemic inflammation and potential organ failure, whereas bacteremia refers to the mere presence of bacteria in the bloodstream without systemic symptoms. Septicemia often results in sepsis, characterized by fever, chills, and hypotension, while bacteremia can be transient and asymptomatic, sometimes occurring after dental procedures. Early diagnosis and treatment differentiate the clinical management, with septicemia requiring aggressive antibiotic therapy and supportive care, unlike bacteremia which may resolve spontaneously.
Signs and Symptoms
Septicemia and bacteremia both involve the presence of bacteria in the bloodstream but differ in severity and clinical presentation. Septicemia typically presents with systemic signs such as high fever, chills, rapid heartbeat, low blood pressure, and signs of organ dysfunction due to the body's inflammatory response. Bacteremia often remains asymptomatic or causes mild symptoms like low-grade fever and malaise unless it progresses to septicemia or other serious infections.
Diagnostic Approaches
Diagnostic approaches for septicemia and bacteremia primarily involve blood cultures to detect and identify the presence of pathogenic bacteria in the bloodstream. In cases of septicemia, additional laboratory tests such as complete blood count, inflammatory markers (e.g., C-reactive protein, procalcitonin), and organ function tests are essential to assess systemic infection severity and possible sepsis progression. Advanced molecular diagnostics like polymerase chain reaction (PCR) and next-generation sequencing (NGS) can enhance pathogen detection sensitivity and speed, aiding timely and accurate differentiation between bacteremia and septicemia.
Treatment Options
Treatment options for septicemia primarily involve aggressive intravenous antibiotic therapy targeting the identified pathogen, along with supportive measures like fluid resuscitation, vasopressors, and organ support in intensive care units. Bacteremia treatment depends on severity and source, often requiring targeted oral or intravenous antibiotics, with close monitoring to prevent progression to septicemia. Early intervention, pathogen identification through blood cultures, and antibiotic susceptibility testing are critical for effective management in both conditions.
Potential Complications
Septicemia can quickly lead to severe systemic infections, causing complications such as septic shock, multi-organ failure, and disseminated intravascular coagulation (DIC). Bacteremia, while sometimes transient and less severe, can progress into infective endocarditis, abscess formation, or transition into septicemia if untreated. Early diagnosis and intervention are critical to preventing the escalation of bacteremia to life-threatening septicemia and its associated complications.
Prevention Strategies
Effective prevention strategies for septicemia and bacteremia center on rigorous infection control practices, including proper hand hygiene, sterile techniques during medical procedures, and timely management of wounds and infections. Vaccinations against common bacterial pathogens, such as Streptococcus pneumoniae and Neisseria meningitidis, reduce the risk of bloodstream infections that can lead to these conditions. Early detection and antibiotic stewardship are crucial to prevent the progression from bacteremia to septicemia, minimizing antibiotic resistance and improving patient outcomes.
Prognosis and Outcomes
Septicemia, characterized by systemic infection and sepsis, generally has a poorer prognosis with higher morbidity and mortality rates compared to bacteremia, which often resolves without severe complications if promptly treated. Outcomes depend on factors such as the patient's immune status, pathogen virulence, and timeliness of antimicrobial therapy. Early recognition and aggressive management significantly improve survival rates in septicemia, whereas bacteremia may remain transient or lead to localized infections if untreated.
Septicemia Infographic
 libterm.com
libterm.com