Hypernatremia is a condition characterized by elevated sodium levels in the blood, often resulting from dehydration, excessive salt intake, or underlying medical issues like kidney dysfunction. Symptoms may include confusion, muscle twitching, and severe thirst, which can escalate to seizures or coma if untreated. Explore the rest of the article to understand hypernatremia's causes, symptoms, treatment, and prevention to protect your health.
Table of Comparison
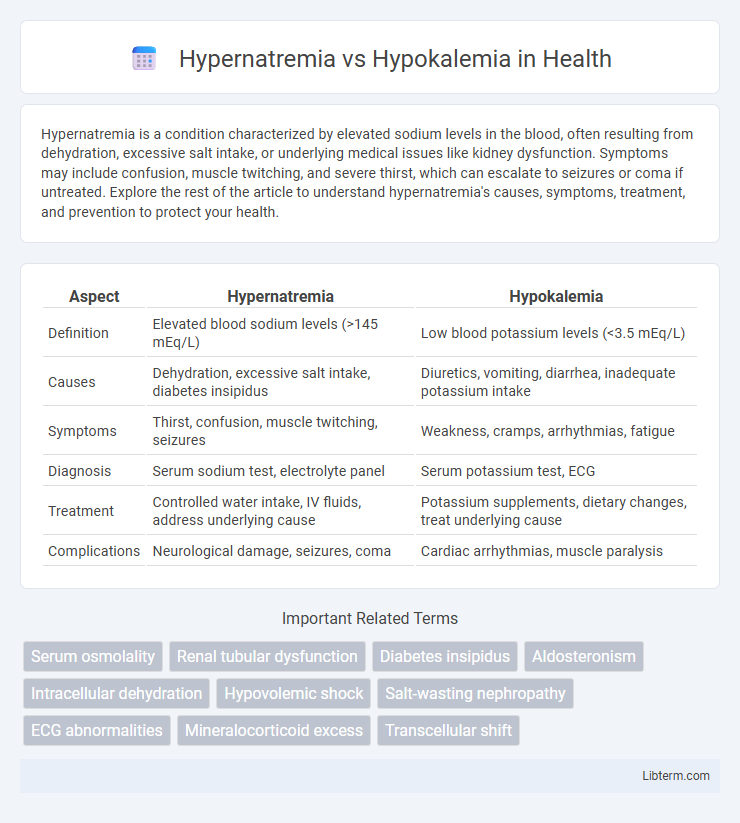
| Aspect | Hypernatremia | Hypokalemia |
|---|---|---|
| Definition | Elevated blood sodium levels (>145 mEq/L) | Low blood potassium levels (<3.5 mEq/L) |
| Causes | Dehydration, excessive salt intake, diabetes insipidus | Diuretics, vomiting, diarrhea, inadequate potassium intake |
| Symptoms | Thirst, confusion, muscle twitching, seizures | Weakness, cramps, arrhythmias, fatigue |
| Diagnosis | Serum sodium test, electrolyte panel | Serum potassium test, ECG |
| Treatment | Controlled water intake, IV fluids, address underlying cause | Potassium supplements, dietary changes, treat underlying cause |
| Complications | Neurological damage, seizures, coma | Cardiac arrhythmias, muscle paralysis |
Introduction to Hypernatremia and Hypokalemia
Hypernatremia is characterized by an elevated serum sodium level exceeding 145 mmol/L, often caused by water loss or excessive sodium intake, leading to cellular dehydration and neurological symptoms. Hypokalemia involves a serum potassium level below 3.5 mmol/L, commonly resulting from diuretic use, gastrointestinal losses, or inadequate potassium intake, and can cause muscle weakness, arrhythmias, and metabolic disturbances. Both electrolyte imbalances critically affect cellular function and necessitate prompt diagnosis and management to prevent serious complications.
Understanding Electrolyte Imbalances
Hypernatremia and hypokalemia are critical electrolyte imbalances affecting sodium and potassium levels in the body, respectively, each disrupting cellular functions and fluid balance. Hypernatremia occurs when serum sodium levels exceed 145 mEq/L, leading to cellular dehydration and neurological symptoms, while hypokalemia, defined by serum potassium levels below 3.5 mEq/L, impairs muscle function and cardiac conduction. Accurate diagnosis and management depend on recognizing the distinct pathophysiological mechanisms, clinical presentations, and electrolyte monitoring to restore homeostasis and prevent complications.
Causes of Hypernatremia
Hypernatremia primarily results from excessive sodium intake, inadequate water consumption, or water loss due to conditions like diabetes insipidus, diarrhea, or excessive sweating. It is characterized by elevated serum sodium levels above 145 mEq/L, leading to cellular dehydration and neurological symptoms. Understanding these causes helps differentiate hypernatremia from hypokalemia, which involves low potassium levels due to factors like diuretic use, vomiting, or chronic kidney disease.
Causes of Hypokalemia
Hypokalemia is primarily caused by excessive potassium loss through the kidneys due to conditions such as diuretic use, hyperaldosteronism, or renal tubular acidosis. Other notable causes include gastrointestinal losses from vomiting, diarrhea, or laxative abuse, as well as inadequate dietary potassium intake and shifts of potassium into cells triggered by insulin or beta-agonists. Unlike hypernatremia, which involves elevated sodium levels often due to water loss or excessive sodium intake, hypokalemia specifically reflects potassium depletion affecting cellular function and muscle activity.
Clinical Manifestations: Hypernatremia vs Hypokalemia
Hypernatremia presents with clinical manifestations such as intense thirst, dry mucous membranes, restlessness, and in severe cases, seizures or coma due to cellular dehydration. Hypokalemia often manifests as muscle weakness, cramps, fatigue, and cardiac arrhythmias due to impaired neuromuscular and cardiac function. Recognizing these distinct symptoms is crucial for timely diagnosis and management of electrolyte imbalances.
Diagnostic Approaches
Hypernatremia diagnosis involves assessing serum sodium levels above 145 mEq/L, combined with evaluating patient history for dehydration, diabetes insipidus, or renal function abnormalities. Hypokalemia diagnosis requires serum potassium measurement below 3.5 mEq/L, alongside ECG changes like U waves, muscle weakness symptoms, and investigation of causes such as diuretic use or gastrointestinal losses. Both conditions necessitate comprehensive electrolyte panels, urine analysis, and clinical examination for accurate differentiation and effective management.
Complications and Health Risks
Hypernatremia can cause severe neurological complications such as seizures, brain swelling, and permanent brain damage due to cellular dehydration and impaired neural function. Hypokalemia increases the risk of cardiac arrhythmias, muscle weakness, and paralysis by disrupting normal electrical conduction and muscle contraction processes. Both electrolyte imbalances require prompt medical intervention to prevent life-threatening outcomes like cardiac arrest or irreversible neurological damage.
Treatment Strategies and Management
Treatment strategies for hypernatremia focus on gradual correction of serum sodium levels using hypotonic fluids such as 5% dextrose in water or half-normal saline to prevent cerebral edema, with close monitoring of electrolytes and patient hydration status. Management of hypokalemia involves potassium replacement through oral or intravenous routes depending on severity, along with addressing underlying causes such as diuretic use or excessive gastrointestinal losses. Continuous cardiac monitoring is essential in severe hypokalemia due to the risk of arrhythmias, and adjustments in magnesium levels may be necessary to facilitate potassium repletion.
Prevention and Monitoring Tips
Preventing hypernatremia involves ensuring adequate hydration and regularly monitoring serum sodium levels, especially in patients with impaired thirst or on diuretics. For hypokalemia, maintaining balanced potassium intake through diet or supplements and frequent electrolyte checks in those on medications like loop diuretics or corticosteroids are key. Continuous monitoring of renal function and ECG changes helps detect electrolyte imbalances early, guiding timely interventions.
Key Differences: Hypernatremia vs Hypokalemia
Hypernatremia is characterized by elevated sodium levels in the blood exceeding 145 mEq/L, leading to cellular dehydration and neurological symptoms, whereas hypokalemia involves low potassium levels below 3.5 mEq/L causing muscle weakness and cardiac arrhythmias. Hypernatremia primarily results from water loss or excessive sodium intake, while hypokalemia often arises due to diuretic use, gastrointestinal losses, or inadequate potassium intake. Management strategies differ significantly; hypernatremia treatment focuses on gradual rehydration with hypotonic fluids, whereas hypokalemia requires potassium supplementation and correction of underlying causes.
Hypernatremia Infographic
 libterm.com
libterm.com