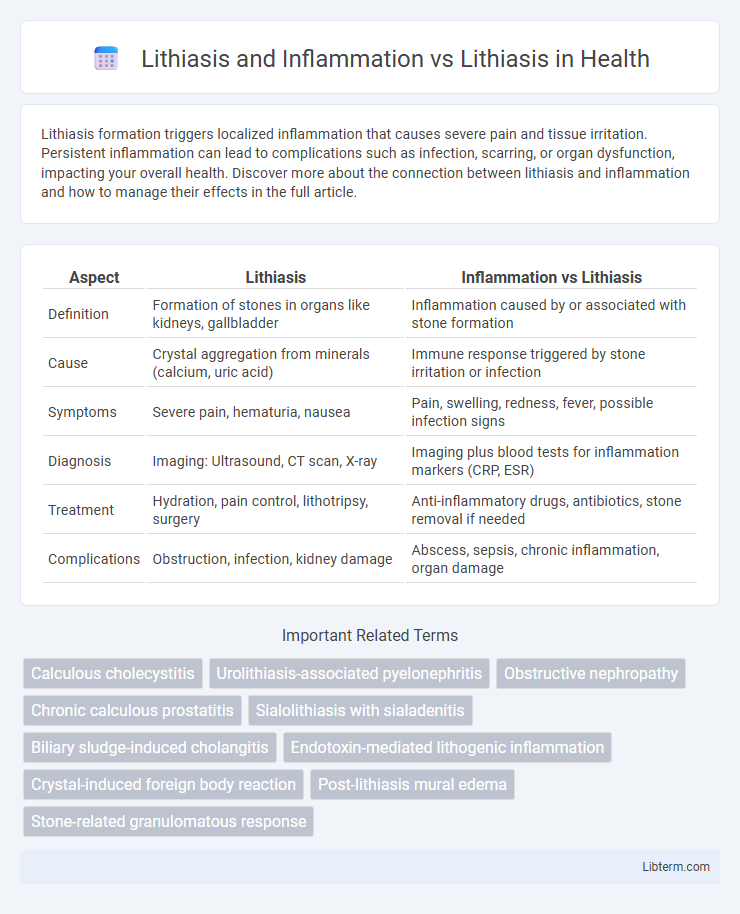
Lithiasis formation triggers localized inflammation that causes severe pain and tissue irritation. Persistent inflammation can lead to complications such as infection, scarring, or organ dysfunction, impacting your overall health. Discover more about the connection between lithiasis and inflammation and how to manage their effects in the full article.
Table of Comparison
| Aspect | Lithiasis | Inflammation vs Lithiasis |
|---|---|---|
| Definition | Formation of stones in organs like kidneys, gallbladder | Inflammation caused by or associated with stone formation |
| Cause | Crystal aggregation from minerals (calcium, uric acid) | Immune response triggered by stone irritation or infection |
| Symptoms | Severe pain, hematuria, nausea | Pain, swelling, redness, fever, possible infection signs |
| Diagnosis | Imaging: Ultrasound, CT scan, X-ray | Imaging plus blood tests for inflammation markers (CRP, ESR) |
| Treatment | Hydration, pain control, lithotripsy, surgery | Anti-inflammatory drugs, antibiotics, stone removal if needed |
| Complications | Obstruction, infection, kidney damage | Abscess, sepsis, chronic inflammation, organ damage |
Understanding Lithiasis: Definition and Types
Lithiasis refers to the formation of stones, or calculi, in organs such as the kidneys, gallbladder, or urinary tract, caused by the accumulation of mineral salts. Understanding lithiasis involves recognizing its main types, including nephrolithiasis (kidney stones), cholelithiasis (gallstones), and urolithiasis (stones in the urinary tract), each varying depending on location and composition like calcium oxalate or cholesterol stones. Inflammation related to lithiasis occurs when these stones irritate tissues, leading to conditions such as pyelonephritis or cholecystitis, which require distinct clinical management from uncomplicated lithiasis.
Inflammation: Mechanisms and Role in Lithiasis
Inflammation plays a pivotal role in the pathogenesis of lithiasis by promoting crystal retention and growth within the urinary tract. The inflammatory response involves the activation of immune cells, release of cytokines, and production of reactive oxygen species, which contribute to tissue damage and facilitate nidus formation for stone development. Understanding the molecular mechanisms linking inflammation and lithiasis offers potential therapeutic targets to prevent stone recurrence and improve patient outcomes.
Lithiasis Without Inflammation: Clinical Features
Lithiasis without inflammation primarily presents with symptoms related to obstruction, such as intermittent colicky pain and hematuria, without signs of infection or systemic inflammatory response. Patients typically exhibit normal white blood cell counts and lack fever, distinguishing it from lithiasis complicated by inflammation where symptoms include severe pain, fever, and elevated inflammatory markers. Imaging techniques like ultrasound and non-contrast CT scans reveal the presence of calculi without adjacent tissue edema or signs of infection, supporting the diagnosis of non-inflammatory lithiasis.
Comparing Lithiasis With and Without Inflammation
Lithiasis with inflammation involves the presence of calculi, such as kidney or gallstones, accompanied by an inflammatory response causing symptoms like pain, swelling, and potential infection. In contrast, lithiasis without inflammation typically presents asymptomatically or with mild discomfort, as the calculi do not trigger significant tissue irritation or immune activity. The prognosis and treatment strategies differ, with inflamed lithiasis often requiring anti-inflammatory medications or surgical intervention to prevent complications like abscess formation or organ damage.
Pathophysiological Connections Between Lithiasis and Inflammation
Lithiasis, characterized by the formation of stones within the urinary or biliary tract, triggers an inflammatory response due to mechanical irritation and obstruction of normal flow. The pathophysiological connection involves activation of immune cells and release of pro-inflammatory cytokines, which exacerbate tissue damage and promote further stone formation. Chronic inflammation alters the local microenvironment, facilitating crystalline aggregation and deposition, thereby perpetuating a cycle between lithiasis and inflammation.
Diagnostic Approaches: Identifying Inflammation in Lithiasis
Diagnostic approaches for identifying inflammation in lithiasis involve advanced imaging techniques such as contrast-enhanced CT scans and MRI, which detect perinephric stranding, wall thickening, and fluid collections indicative of inflammation. Laboratory markers including elevated C-reactive protein (CRP) and leukocytosis support the diagnosis of inflammatory complications in patients with lithiasis. Combining clinical evaluation with these imaging and biochemical parameters enhances accuracy in differentiating simple lithiasis from lithiasis with associated inflammatory processes.
Impact of Inflammation on Lithiasis Progression
Inflammation accelerates lithiasis progression by promoting stone nucleation and growth through inflammatory mediators and oxidative stress. It alters urinary composition, reducing natural inhibitors of crystallization and increasing calcium and oxalate concentration. Chronic inflammation also damages renal tissues, exacerbating stone formation and recurrence rates.
Treatment Strategies: Managing Lithiasis With Inflammatory Components
Treatment strategies for lithiasis with inflammatory components focus on addressing both the obstructive stones and the underlying inflammation to prevent complications like infection or tissue damage. Anti-inflammatory medications combined with targeted antibiotic therapy, when infection is present, help reduce swelling and manage pain alongside lithotripsy or surgical stone removal. Early intervention and coordinated care improve patient outcomes by minimizing recurrent inflammation and promoting complete stone clearance.
Prognosis: Outcomes in Inflammatory vs Non-Inflammatory Lithiasis
Inflammatory lithiasis often results in a poorer prognosis due to increased risks of infection, tissue damage, and recurrence compared to non-inflammatory lithiasis. Outcomes in inflammatory cases may include chronic pain, abscess formation, or stricter complications, necessitating more aggressive treatments and prolonged monitoring. Non-inflammatory lithiasis generally presents with fewer complications, enabling better recovery and a reduced likelihood of long-term morbidity.
Preventive Measures: Reducing Risk of Inflammatory Lithiasis
Preventive measures for inflammatory lithiasis focus on reducing factors that promote infection and stone formation, such as maintaining proper hydration to dilute urine and prevent crystal aggregation. Regular medical check-ups to detect and treat urinary tract infections promptly help minimize chronic inflammation that contributes to stone development. Dietary adjustments limiting salt and oxalate intake alongside avoiding urinary stasis through physical activity reduce the risk of both lithiasis and subsequent inflammatory complications.
Lithiasis and Inflammation Infographic
 libterm.com
libterm.com