Stroke is a medical emergency that occurs when the blood supply to part of the brain is interrupted or reduced, causing brain cells to die. Recognizing the early symptoms and seeking immediate treatment is critical to minimizing long-term damage and improving recovery outcomes. Learn more about the signs, risk factors, and prevention methods to protect your health in the rest of this article.
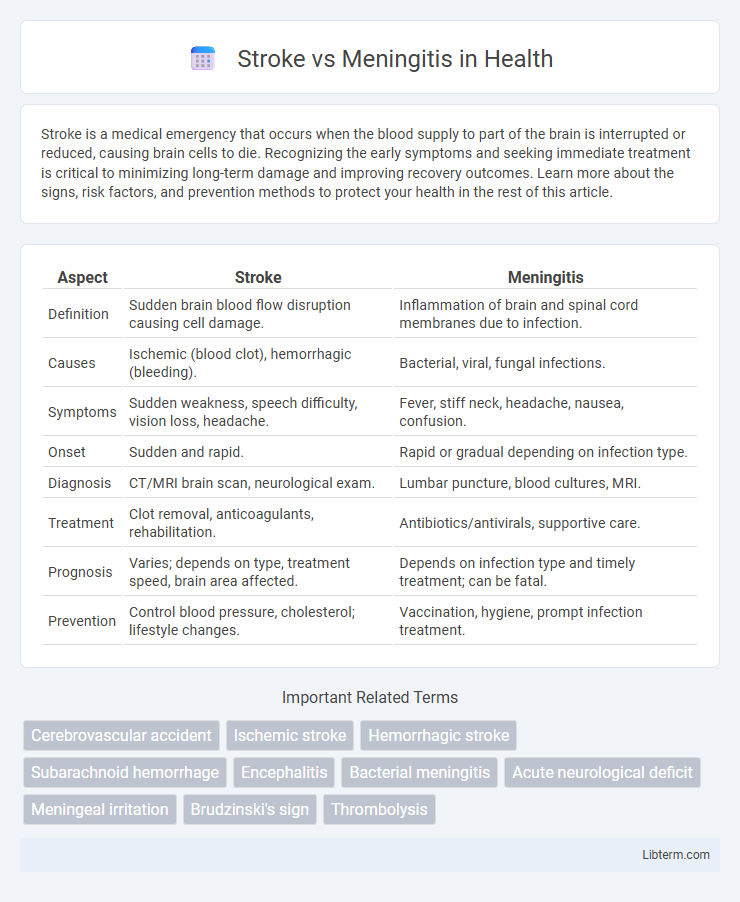
Table of Comparison
| Aspect | Stroke | Meningitis |
|---|---|---|
| Definition | Sudden brain blood flow disruption causing cell damage. | Inflammation of brain and spinal cord membranes due to infection. |
| Causes | Ischemic (blood clot), hemorrhagic (bleeding). | Bacterial, viral, fungal infections. |
| Symptoms | Sudden weakness, speech difficulty, vision loss, headache. | Fever, stiff neck, headache, nausea, confusion. |
| Onset | Sudden and rapid. | Rapid or gradual depending on infection type. |
| Diagnosis | CT/MRI brain scan, neurological exam. | Lumbar puncture, blood cultures, MRI. |
| Treatment | Clot removal, anticoagulants, rehabilitation. | Antibiotics/antivirals, supportive care. |
| Prognosis | Varies; depends on type, treatment speed, brain area affected. | Depends on infection type and timely treatment; can be fatal. |
| Prevention | Control blood pressure, cholesterol; lifestyle changes. | Vaccination, hygiene, prompt infection treatment. |
Understanding Stroke and Meningitis: Key Differences
Stroke occurs when blood flow to the brain is interrupted, leading to sudden neurological deficits, while meningitis is an inflammation of the protective membranes surrounding the brain and spinal cord, typically caused by infection. Key differences include the onset of symptoms--stroke often presents with sudden weakness or speech difficulties, whereas meningitis features fever, headache, and neck stiffness. Accurate diagnosis through imaging for stroke and cerebrospinal fluid analysis for meningitis is crucial for effective treatment and improved patient outcomes.
Causes and Risk Factors of Stroke vs Meningitis
Stroke primarily results from interrupted blood supply to the brain, often caused by ischemic factors such as blood clots or hemorrhagic events like ruptured arteries, with significant risk factors including hypertension, smoking, diabetes, and high cholesterol. Meningitis is caused by inflammation of the protective membranes around the brain and spinal cord, typically triggered by bacterial, viral, or fungal infections, with risk factors encompassing close living conditions, weakened immune systems, and age extremes. Understanding these distinct etiologies and risk profiles is critical for targeted prevention and early intervention strategies.
Primary Symptoms: Stroke vs Meningitis
Stroke primarily presents with sudden numbness or weakness, especially on one side of the body, confusion, trouble speaking, or loss of balance. Meningitis symptoms usually start with severe headache, high fever, stiff neck, and sensitivity to light. Both conditions require immediate medical evaluation but differ in neurological deficits and infection signs.
How Each Condition Affects the Brain
Stroke occurs when blood flow to a part of the brain is interrupted or reduced, causing brain cells to die due to lack of oxygen and nutrients, leading to localized brain damage. Meningitis is the inflammation of the protective membranes covering the brain and spinal cord, usually caused by infection, which can lead to increased intracranial pressure, brain swelling, and damage to the central nervous system. Both conditions disrupt normal brain function but differ in their pathological mechanisms and immediate impact on brain tissue.
Diagnostic Procedures for Stroke and Meningitis
Diagnostic procedures for stroke primarily involve neuroimaging techniques such as computed tomography (CT) scans and magnetic resonance imaging (MRI), which help identify ischemic or hemorrhagic brain injury. For meningitis, diagnosis relies on cerebrospinal fluid (CSF) analysis obtained through lumbar puncture, alongside blood cultures and PCR testing to detect infectious agents. Early and accurate differentiation between stroke and meningitis is critical, as imaging guides acute stroke interventions while CSF profiles determine the appropriate antimicrobial or supportive therapy for meningitis.
Immediate Treatment Options
Immediate treatment for stroke involves restoring blood flow through thrombolytic therapy using tissue plasminogen activator (tPA) within the critical 3 to 4.5-hour window from symptom onset, or mechanical thrombectomy for eligible ischemic stroke patients. Meningitis treatment requires prompt administration of high-dose intravenous antibiotics tailored to the causative pathogen, alongside corticosteroids to reduce inflammation and potential neurological damage. Rapid diagnosis via imaging and lumbar puncture guides targeted therapy to minimize long-term complications in both conditions.
Long-term Outcomes and Complications
Stroke often results in long-term neurological deficits such as paralysis, speech difficulties, and cognitive impairments, with complications including recurrent strokes, post-stroke epilepsy, and depression. Meningitis survivors may experience chronic complications like hearing loss, learning disabilities, seizures, and hydrocephalus, with the severity largely dependent on the causative pathogen and timing of treatment. Both conditions require comprehensive rehabilitation and ongoing medical management to address persistent disabilities and improve quality of life.
Preventive Measures for Stroke and Meningitis
Preventive measures for stroke include controlling high blood pressure, maintaining a healthy diet rich in fruits and vegetables, regular physical activity, avoiding smoking, and managing diabetes and cholesterol levels. Meningitis prevention involves vaccination against common bacterial strains such as Neisseria meningitidis and Streptococcus pneumoniae, practicing good hygiene like frequent handwashing, and avoiding close contact with infected individuals. Early detection and timely medical intervention significantly reduce the risk and severity of both stroke and meningitis.
Patient Recovery: Rehabilitation and Support
Patient recovery from stroke involves intensive rehabilitation focusing on physical, occupational, and speech therapy to regain lost functions and improve quality of life, often requiring months to years of tailored support. Meningitis recovery centers on addressing neurological complications and potential cognitive impairments through specialized therapies and ongoing medical monitoring, especially if bacterial infection caused brain inflammation. Both conditions necessitate comprehensive support systems including psychological counseling and caregiver involvement to optimize long-term outcomes and prevent recurrence.
When to Seek Emergency Medical Help
Seek emergency medical help immediately if you experience sudden weakness, numbness, difficulty speaking, or facial drooping, as these are classic signs of a stroke requiring urgent intervention to restore blood flow and minimize brain damage. For meningitis, emergency care is critical when symptoms like high fever, severe headache, neck stiffness, confusion, or sensitivity to light appear, indicating a potential life-threatening infection of the brain's protective membranes. Rapid diagnosis and treatment in both conditions can drastically improve outcomes and reduce the risk of long-term complications.
Stroke Infographic
 libterm.com
libterm.com