Hypocalcemia occurs when calcium levels in the blood drop below normal, leading to symptoms like muscle cramps, tingling, and fatigue. Causes include vitamin D deficiency, kidney disease, or parathyroid gland dysfunction, all of which disrupt calcium balance. Discover detailed insights on symptoms, causes, and effective treatments by reading the rest of the article.
Table of Comparison
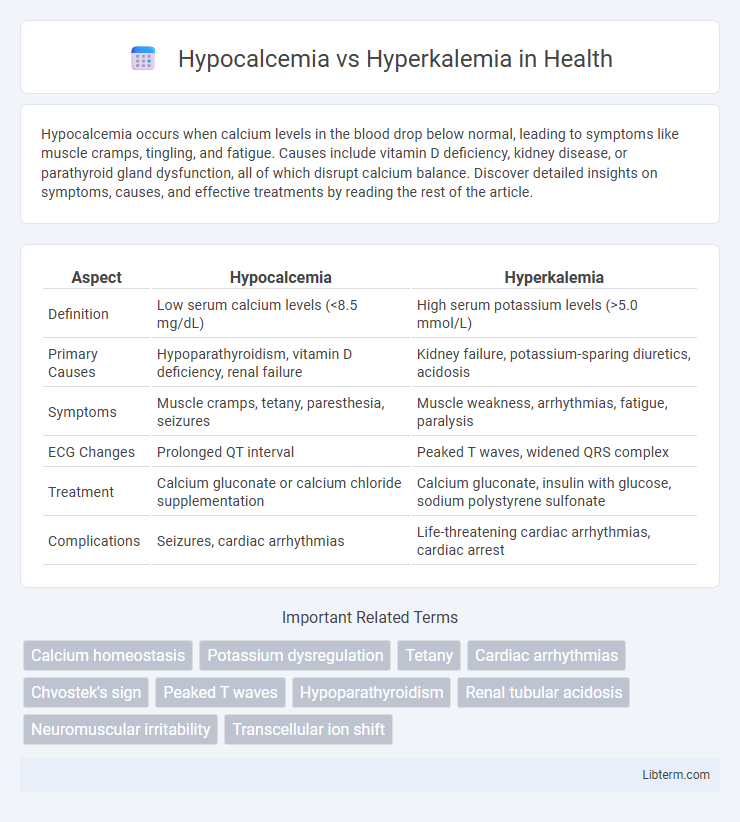
| Aspect | Hypocalcemia | Hyperkalemia |
|---|---|---|
| Definition | Low serum calcium levels (<8.5 mg/dL) | High serum potassium levels (>5.0 mmol/L) |
| Primary Causes | Hypoparathyroidism, vitamin D deficiency, renal failure | Kidney failure, potassium-sparing diuretics, acidosis |
| Symptoms | Muscle cramps, tetany, paresthesia, seizures | Muscle weakness, arrhythmias, fatigue, paralysis |
| ECG Changes | Prolonged QT interval | Peaked T waves, widened QRS complex |
| Treatment | Calcium gluconate or calcium chloride supplementation | Calcium gluconate, insulin with glucose, sodium polystyrene sulfonate |
| Complications | Seizures, cardiac arrhythmias | Life-threatening cardiac arrhythmias, cardiac arrest |
Introduction to Hypocalcemia and Hyperkalemia
Hypocalcemia is defined by abnormally low levels of calcium in the blood, which can lead to muscle cramps, tetany, and cardiac arrhythmias due to impaired neuromuscular function. Hyperkalemia involves elevated potassium levels that disrupt normal cellular electrical activity, potentially causing muscle weakness, paralysis, and life-threatening cardiac arrhythmias. Both electrolyte imbalances reflect critical disturbances in mineral homeostasis requiring prompt diagnosis and intervention to prevent severe complications.
Definition and Overview
Hypocalcemia is a condition characterized by abnormally low levels of calcium in the blood, typically below 8.5 mg/dL, affecting neuromuscular function and cardiac stability. Hyperkalemia refers to elevated potassium levels in the bloodstream, usually above 5.0 mEq/L, which can disrupt cardiac rhythm and muscle function. Both electrolyte imbalances require prompt diagnosis and tailored treatment to prevent serious complications.
Etiology: Causes of Hypocalcemia and Hyperkalemia
Hypocalcemia is primarily caused by vitamin D deficiency, hypoparathyroidism, chronic kidney disease, and magnesium deficiency, leading to impaired calcium absorption or increased calcium loss. Hyperkalemia arises mainly from renal failure, medications such as potassium-sparing diuretics, adrenal insufficiency, and cellular injury releasing intracellular potassium into the bloodstream. Both conditions reflect distinct disturbances in electrolyte homeostasis with varying etiologies impacting calcium and potassium levels respectively.
Pathophysiology: How Each Condition Affects the Body
Hypocalcemia results from low serum calcium levels, impairing neuromuscular function by increasing neuronal excitability and causing muscle spasms or tetany due to destabilization of the resting membrane potential. Hyperkalemia involves elevated serum potassium, which disrupts cardiac conduction and muscle function by reducing the resting membrane potential and impairing action potential propagation, potentially leading to life-threatening arrhythmias. Both conditions alter ion gradients critical for cellular excitability but affect different ions and tissues, resulting in distinct clinical manifestations and risks.
Clinical Manifestations: Signs and Symptoms
Hypocalcemia presents with neuromuscular irritability, including muscle cramps, tetany, and positive Chvostek's and Trousseau's signs, alongside symptoms like paresthesia and seizures. Hyperkalemia primarily affects cardiac and neuromuscular function, causing muscle weakness, fatigue, and life-threatening arrhythmias such as peaked T waves and widened QRS complexes on ECG. Both electrolyte imbalances require prompt recognition of distinct clinical manifestations to prevent severe complications.
Diagnostic Differences
Hypocalcemia is diagnosed primarily through serum calcium levels below 8.5 mg/dL, often accompanied by symptoms such as tetany and muscle cramps, while hyperkalemia is identified by serum potassium levels exceeding 5.0 mEq/L, which may cause cardiac arrhythmias detectable on an ECG. Diagnostic tests for hypocalcemia often include measuring ionized calcium and parathyroid hormone levels, whereas hyperkalemia diagnosis emphasizes potassium assays and renal function assessments to determine underlying causes. Electrocardiographic changes like prolonged QT interval suggest hypocalcemia, contrasting with peaked T waves characteristic of hyperkalemia.
Laboratory Findings and Key Biomarkers
Hypocalcemia presents with low serum calcium levels typically below 8.5 mg/dL, decreased ionized calcium, and elevated parathyroid hormone (PTH) as a compensatory response. Hyperkalemia is characterized by elevated serum potassium levels exceeding 5.0 mEq/L, along with potential EKG changes such as peaked T waves, and may show normal calcium and PTH levels. Key biomarkers distinguishing hypocalcemia include low total and ionized calcium and high PTH, while hyperkalemia is identified primarily by elevated potassium concentration and characteristic cardiac conduction abnormalities.
Management and Treatment Strategies
Management of hypocalcemia involves calcium supplementation either orally or intravenously, alongside addressing underlying causes such as vitamin D deficiency or hypoparathyroidism. Hyperkalemia treatment prioritizes stabilizing cardiac membranes with intravenous calcium gluconate, followed by measures to shift potassium intracellularly using insulin and glucose, and enhancing potassium elimination through diuretics, potassium binders, or dialysis. Continuous monitoring of electrolyte levels and cardiac function is essential in both conditions to prevent life-threatening complications.
Potential Complications and Prognosis
Hypocalcemia can lead to neuromuscular irritability, tetany, seizures, and cardiac arrhythmias, significantly impacting patient prognosis without timely intervention. Hyperkalemia primarily causes life-threatening cardiac arrhythmias, including ventricular fibrillation and cardiac arrest, posing an acute emergency with high mortality risk. Both electrolyte imbalances require prompt diagnosis and management to prevent severe complications and improve long-term outcomes.
Prevention and Patient Education
Effective prevention of hypocalcemia involves maintaining adequate dietary calcium and vitamin D intake, monitoring serum calcium levels in high-risk patients, and educating patients about symptoms such as muscle cramps and tingling. For hyperkalemia, preventing excess potassium includes managing potassium-rich food intake, monitoring kidney function, and educating patients on signs like muscle weakness and irregular heartbeat. Both conditions require patient education on medication adherence, such as avoiding certain diuretics for hypocalcemia or potassium-sparing drugs for hyperkalemia, to reduce risk and ensure timely intervention.
Hypocalcemia Infographic
 libterm.com
libterm.com