Hemolytic anemia occurs when red blood cells are destroyed faster than the body can replace them, leading to symptoms like fatigue, jaundice, and shortness of breath. Causes range from inherited conditions to autoimmune disorders, infections, and certain medications. Discover how hemolytic anemia affects your health and learn about diagnosis, treatment options, and management strategies in the full article.
Table of Comparison
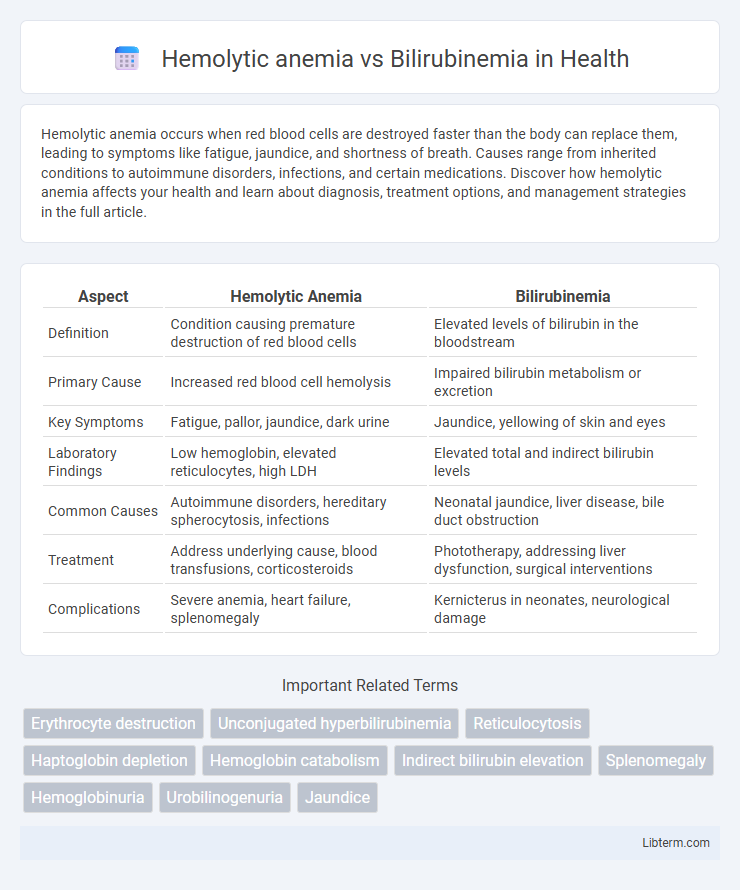
| Aspect | Hemolytic Anemia | Bilirubinemia |
|---|---|---|
| Definition | Condition causing premature destruction of red blood cells | Elevated levels of bilirubin in the bloodstream |
| Primary Cause | Increased red blood cell hemolysis | Impaired bilirubin metabolism or excretion |
| Key Symptoms | Fatigue, pallor, jaundice, dark urine | Jaundice, yellowing of skin and eyes |
| Laboratory Findings | Low hemoglobin, elevated reticulocytes, high LDH | Elevated total and indirect bilirubin levels |
| Common Causes | Autoimmune disorders, hereditary spherocytosis, infections | Neonatal jaundice, liver disease, bile duct obstruction |
| Treatment | Address underlying cause, blood transfusions, corticosteroids | Phototherapy, addressing liver dysfunction, surgical interventions |
| Complications | Severe anemia, heart failure, splenomegaly | Kernicterus in neonates, neurological damage |
Understanding Hemolytic Anemia: Definition and Causes
Hemolytic anemia is a condition characterized by the premature destruction of red blood cells, leading to a decreased oxygen-carrying capacity in the bloodstream. Common causes include autoimmune diseases, genetic disorders like sickle cell anemia, infections, certain medications, and exposure to toxins. This accelerated red blood cell breakdown results in an increased release of bilirubin, often causing bilirubinemia, which manifests as elevated bilirubin levels in the blood.
What is Bilirubinemia? Types and Mechanisms
Bilirubinemia refers to elevated levels of bilirubin in the blood, often resulting from increased red blood cell destruction, impaired bilirubin conjugation, or biliary obstruction. There are two main types: unconjugated (indirect) bilirubinemia caused by excessive hemolysis or impaired hepatic uptake, and conjugated (direct) bilirubinemia resulting from hepatocellular damage or bile duct obstruction. Mechanisms involve hemolytic anemia increasing bilirubin production, defective liver enzymes reducing conjugation, or cholestasis impairing bilirubin excretion.
Key Differences Between Hemolytic Anemia and Bilirubinemia
Hemolytic anemia is a condition characterized by the premature destruction of red blood cells, leading to decreased hemoglobin levels and symptoms like fatigue and pallor. Bilirubinemia refers to elevated levels of bilirubin in the blood, often causing jaundice, and results from increased red blood cell breakdown or liver dysfunction. The key difference lies in hemolytic anemia directly affecting red blood cell lifespan and production, whereas bilirubinemia is a biochemical marker indicating impaired bilirubin metabolism or clearance.
Pathophysiology: How Hemolysis Leads to Bilirubin Increase
Hemolytic anemia causes the premature destruction of red blood cells, releasing large amounts of hemoglobin into the bloodstream that is subsequently broken down into heme and globin. Heme is converted into biliverdin and then into unconjugated bilirubin, overwhelming the liver's capacity to conjugate and excrete it. This accumulation of unconjugated bilirubin results in bilirubinemia, manifesting clinically with jaundice and elevated serum bilirubin levels.
Clinical Manifestations: Symptoms of Both Conditions
Hemolytic anemia presents with symptoms such as fatigue, pallor, jaundice, dark urine, and an enlarged spleen due to the rapid destruction of red blood cells. Bilirubinemia manifests primarily with jaundice, yellowing of the skin and eyes, and dark-colored urine caused by elevated bilirubin levels in the bloodstream. Both conditions share jaundice as a common clinical feature but differ in underlying mechanisms and associated symptoms like anemia and splenomegaly seen in hemolytic anemia.
Diagnostic Approaches: Laboratory Tests and Biomarkers
Hemolytic anemia diagnosis relies on laboratory tests such as a complete blood count (CBC), reticulocyte count, peripheral blood smear, and elevated lactate dehydrogenase (LDH) levels, alongside reduced haptoglobin and increased indirect bilirubin. Bilirubinemia is primarily assessed by measuring total, direct, and indirect bilirubin concentrations in serum, with marked indirect hyperbilirubinemia often indicative of hemolysis. Biomarkers like Coombs test for autoimmune hemolysis and serum unconjugated bilirubin help differentiate hemolytic anemia from other causes of elevated bilirubin.
Common Triggers and Risk Factors for Hemolytic Anemia and Bilirubinemia
Hemolytic anemia commonly arises from triggers such as autoimmune disorders, infections like malaria, certain medications, and inherited conditions including sickle cell disease and G6PD deficiency. Bilirubinemia often occurs due to excessive red blood cell breakdown, liver dysfunction, or bile duct obstruction, with risk factors including neonatal jaundice, hemolysis, and genetic disorders like Gilbert's syndrome. Both conditions share risk factors related to increased red blood cell destruction but differ in the specific underlying causes and affected organs.
Management Strategies: Treatment Options for Each Condition
Hemolytic anemia management centers on treating the underlying cause and may include corticosteroids, immunosuppressive therapy, blood transfusions, or splenectomy in severe cases. Bilirubinemia, particularly neonatal jaundice, is commonly managed using phototherapy to reduce serum bilirubin levels and, in extreme cases, exchange transfusion to prevent kernicterus. Both conditions require regular monitoring of hemoglobin and bilirubin levels to guide treatment efficacy and prevent complications.
Complications Arising from Hemolytic Anemia vs Bilirubinemia
Hemolytic anemia often leads to complications such as splenomegaly, gallstones, and severe fatigue due to the accelerated destruction of red blood cells and consequent chronic anemia. Bilirubinemia, characterized by elevated bilirubin levels in the blood, primarily results in jaundice and can cause kernicterus in newborns if untreated. Both conditions risk causing significant organ damage, but hemolytic anemia complicates oxygen delivery, whereas bilirubinemia mainly impacts liver function and neurological health.
Prognosis and Long-term Outcomes: What Patients Should Know
Hemolytic anemia prognosis varies widely depending on the underlying cause but often requires ongoing management to prevent complications such as organ damage or severe anemia. Bilirubinemia, primarily indicative of jaundice from excess bilirubin, usually resolves with treatment of the underlying cause but can lead to kernicterus or neurological damage if untreated in newborns. Patients should understand the importance of early diagnosis and tailored treatment plans to improve long-term outcomes and reduce the risk of chronic health issues.
Hemolytic anemia Infographic
 libterm.com
libterm.com