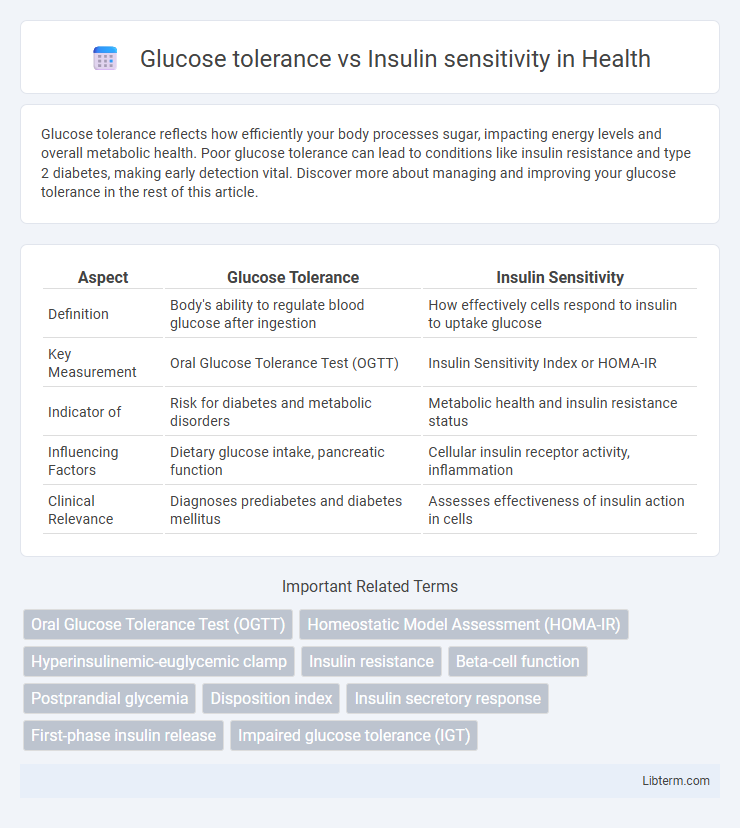
Glucose tolerance reflects how efficiently your body processes sugar, impacting energy levels and overall metabolic health. Poor glucose tolerance can lead to conditions like insulin resistance and type 2 diabetes, making early detection vital. Discover more about managing and improving your glucose tolerance in the rest of this article.
Table of Comparison
| Aspect | Glucose Tolerance | Insulin Sensitivity |
|---|---|---|
| Definition | Body's ability to regulate blood glucose after ingestion | How effectively cells respond to insulin to uptake glucose |
| Key Measurement | Oral Glucose Tolerance Test (OGTT) | Insulin Sensitivity Index or HOMA-IR |
| Indicator of | Risk for diabetes and metabolic disorders | Metabolic health and insulin resistance status |
| Influencing Factors | Dietary glucose intake, pancreatic function | Cellular insulin receptor activity, inflammation |
| Clinical Relevance | Diagnoses prediabetes and diabetes mellitus | Assesses effectiveness of insulin action in cells |
Introduction to Glucose Tolerance and Insulin Sensitivity
Glucose tolerance measures the body's efficiency in clearing glucose from the bloodstream after ingestion, indicating how well the pancreas and cells respond to sugar intake. Insulin sensitivity refers to how responsive cells are to insulin, facilitating glucose uptake and maintaining blood sugar levels within a healthy range. Both metrics are critical in diagnosing and managing metabolic conditions such as diabetes and insulin resistance.
Defining Glucose Tolerance: Key Concepts
Glucose tolerance refers to the body's ability to regulate blood glucose levels after ingesting carbohydrates, primarily measured through an oral glucose tolerance test (OGTT). It assesses how efficiently glucose is cleared from the bloodstream, indicating pancreatic beta-cell function and insulin response. Impaired glucose tolerance is a critical marker for prediabetes and increased risk of type 2 diabetes mellitus.
Understanding Insulin Sensitivity: Essential Insights
Insulin sensitivity refers to how effectively the body's cells respond to insulin, facilitating glucose uptake and maintaining blood sugar levels. High insulin sensitivity allows for efficient glucose metabolism, reducing the risk of type 2 diabetes and metabolic syndrome. Understanding insulin sensitivity involves analyzing factors like diet, physical activity, and genetic predisposition that influence cellular response to insulin.
Physiological Mechanisms Behind Glucose Tolerance
Glucose tolerance depends on the efficient uptake of glucose by tissues, primarily skeletal muscle and adipose tissue, mediated by insulin-stimulated GLUT4 translocation to the cell membrane. Insulin sensitivity reflects the responsiveness of cells to insulin, influencing glucose uptake and hepatic glucose production suppression. Key physiological mechanisms involve pancreatic b-cell insulin secretion, insulin receptor signaling pathways, and glucose transporter activity, which collectively maintain blood glucose homeostasis.
Cellular and Molecular Basis of Insulin Sensitivity
Insulin sensitivity at the cellular level is primarily determined by the efficiency of insulin receptor signaling pathways, including the activation of insulin receptor substrate (IRS) proteins and downstream effectors such as phosphoinositide 3-kinase (PI3K) and protein kinase B (Akt). Cellular glucose uptake is facilitated by the translocation of glucose transporter 4 (GLUT4) to the plasma membrane, a process tightly regulated by insulin signaling cascades. Impairments in these molecular mechanisms disrupt insulin sensitivity, contributing to impaired glucose tolerance and metabolic disorders like type 2 diabetes.
Diagnostic Tests: OGTT vs. Insulin Sensitivity Testing
The Oral Glucose Tolerance Test (OGTT) measures the body's ability to metabolize glucose by assessing blood sugar levels at set intervals after glucose ingestion, providing direct insight into glucose tolerance. Insulin sensitivity testing, such as the hyperinsulinemic-euglycemic clamp or HOMA-IR calculation, evaluates how effectively insulin facilitates glucose uptake at the cellular level, indicating insulin efficiency rather than glucose processing alone. These diagnostic tests differ in focus: OGTT reflects overall glucose tolerance and potential diabetes risk, while insulin sensitivity tests offer detailed analysis of insulin action and resistance.
Factors Affecting Glucose Tolerance and Insulin Sensitivity
Factors affecting glucose tolerance include genetic predisposition, beta-cell function, and dietary carbohydrate intake, which influence how effectively the body manages blood glucose levels. Insulin sensitivity is modulated by physical activity, body fat distribution, especially visceral adiposity, and inflammatory markers that impact cellular insulin receptor activity. Both glucose tolerance and insulin sensitivity are also affected by age, hormonal fluctuations, and medications such as glucocorticoids or thiazolidinediones.
Clinical Implications: Diabetes Risk and Metabolic Health
Impaired glucose tolerance indicates how effectively the body processes glucose after ingestion, serving as a crucial predictor of diabetes risk and potential progression to type 2 diabetes. Insulin sensitivity reflects how responsive cells are to insulin, influencing metabolic health and the ability to maintain normal blood sugar levels. Clinically, assessing both glucose tolerance and insulin sensitivity provides a comprehensive understanding of an individual's diabetes risk and guides targeted interventions to improve metabolic outcomes.
Lifestyle Interventions for Improving Both Parameters
Lifestyle interventions such as regular physical activity, a balanced diet rich in whole grains, fiber, and low-glycemic index foods significantly improve glucose tolerance and insulin sensitivity by enhancing cellular glucose uptake and reducing insulin resistance. Weight management through calorie-controlled nutrition and increased aerobic and resistance exercise reduces visceral fat, a key factor in impaired glucose metabolism and insulin signaling. Consistent lifestyle changes not only stabilize blood glucose levels but also optimize insulin response, lowering the risk of type 2 diabetes and metabolic syndrome.
Summary: Comparing Glucose Tolerance and Insulin Sensitivity
Glucose tolerance measures the body's ability to clear glucose from the bloodstream after a carbohydrate load, often assessed by the oral glucose tolerance test (OGTT). Insulin sensitivity refers to how responsive cells are to insulin's effects in facilitating glucose uptake, a critical factor in maintaining normal blood sugar levels. While both are interrelated, impaired insulin sensitivity (insulin resistance) can lead to reduced glucose tolerance, increasing the risk of type 2 diabetes and metabolic syndrome.
Glucose tolerance Infographic
 libterm.com
libterm.com