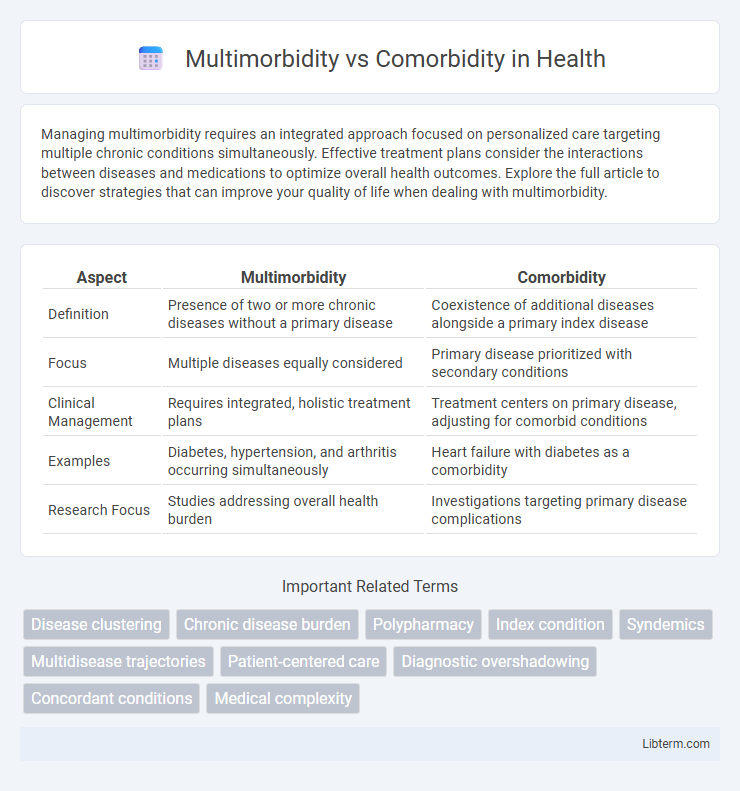
Managing multimorbidity requires an integrated approach focused on personalized care targeting multiple chronic conditions simultaneously. Effective treatment plans consider the interactions between diseases and medications to optimize overall health outcomes. Explore the full article to discover strategies that can improve your quality of life when dealing with multimorbidity.
Table of Comparison
| Aspect | Multimorbidity | Comorbidity |
|---|---|---|
| Definition | Presence of two or more chronic diseases without a primary disease | Coexistence of additional diseases alongside a primary index disease |
| Focus | Multiple diseases equally considered | Primary disease prioritized with secondary conditions |
| Clinical Management | Requires integrated, holistic treatment plans | Treatment centers on primary disease, adjusting for comorbid conditions |
| Examples | Diabetes, hypertension, and arthritis occurring simultaneously | Heart failure with diabetes as a comorbidity |
| Research Focus | Studies addressing overall health burden | Investigations targeting primary disease complications |
Understanding Multimorbidity: Definition and Scope
Multimorbidity refers to the presence of two or more chronic conditions simultaneously in an individual, without a primary index disease, distinguishing it from comorbidity, which revolves around additional diseases co-occurring with a primary condition. Understanding multimorbidity involves recognizing its complex interactions, higher prevalence in aging populations, and significant impact on healthcare utilization and patient quality of life. The scope of multimorbidity encompasses integrated care approaches and tailored interventions to manage this multifaceted health challenge effectively.
Comorbidity Explained: Meaning and Context
Comorbidity refers to the presence of one or more additional diseases or disorders co-occurring with a primary disease, often influencing diagnosis, treatment, and prognosis. Unlike multimorbidity, which indicates multiple conditions without a primary focus, comorbidity emphasizes the relationship between a central illness and its simultaneous secondary conditions. This concept is crucial in clinical settings for tailoring comprehensive care plans and understanding the complexity of patient health status.
Key Differences Between Multimorbidity and Comorbidity
Multimorbidity refers to the presence of two or more chronic conditions occurring simultaneously in a patient without one being the primary disease, whereas comorbidity describes additional diseases coexisting with a primary index disease. In multimorbidity, no single condition takes precedence, highlighting the complexity of managing multiple health issues collectively, while comorbidity emphasizes the influence of secondary conditions on the primary illness's prognosis and treatment. Understanding these distinctions is crucial for clinical decision-making and designing patient-centered care strategies tailored to diverse health profiles.
Epidemiology: Prevalence of Multimorbidity vs Comorbidity
Multimorbidity, defined as the coexistence of two or more chronic conditions in an individual, has a higher prevalence in aging populations, affecting approximately 65% of adults aged 65 and older globally. In contrast, comorbidity, which refers to the presence of one or more additional diseases co-occurring with a primary index disease, is often reported in up to 30% of patients within specific clinical cohorts, such as those with diabetes or cardiovascular disease. Epidemiological data indicate that multimorbidity represents a broader and more complex healthcare challenge, with prevalence rates increasing significantly with socioeconomic deprivation and regional health disparities.
Impacts on Patient Care and Clinical Management
Multimorbidity, characterized by the coexistence of multiple chronic conditions without a single index disease, significantly complicates patient care by requiring holistic, individualized treatment plans that address overlapping pathologies and potential drug interactions. In contrast, comorbidity typically refers to additional diseases co-occurring with a primary index condition, often leading clinicians to prioritize the primary illness while managing secondary conditions. Effective clinical management for multimorbidity demands integrated care approaches and interdisciplinary collaboration to optimize health outcomes and reduce healthcare utilization, whereas comorbidity management may focus more on controlling the primary disease alongside supplementary treatments.
Diagnostic Challenges: Identifying Multiple Conditions
Multimorbidity involves the coexistence of two or more chronic conditions without a primary index disease, complicating diagnostic processes due to overlapping symptoms and the absence of a clear hierarchy. Comorbidity refers to the presence of one or more additional diseases co-occurring with a primary condition, allowing clinicians to prioritize diagnosis based on the index disease. Diagnostic challenges in multimorbidity stem from the need to evaluate multiple interrelated conditions simultaneously, increasing the complexity of clinical assessments and treatment planning.
Risk Factors and Causes: What Leads to Multimorbidity and Comorbidity?
Multimorbidity involves the simultaneous presence of multiple chronic diseases without a primary index condition, while comorbidity refers to additional diseases occurring alongside a primary illness. Risk factors for both include age, genetic predisposition, lifestyle behaviors such as smoking and physical inactivity, and socioeconomic status. Chronic inflammation, environmental exposures, and poor access to healthcare contribute significantly to the development of multimorbidity and comorbidity.
Treatment Strategies: Integrated vs Disease-Specific Approaches
Multimorbidity requires integrated treatment strategies that address multiple chronic conditions simultaneously, emphasizing coordinated care plans to improve overall patient outcomes and reduce medication conflicts. Comorbidity treatment often follows disease-specific approaches targeting a primary condition alongside secondary illnesses, which can lead to fragmented care and increased risk of adverse effects. Optimizing management through holistic frameworks and patient-centered models enhances effectiveness for multimorbidity, while disease-specific protocols may be insufficient for complex cases involving multiple overlapping disorders.
Health Policy Implications for Multimorbid and Comorbid Patients
Health policy must address the distinct needs of patients with multimorbidity, who experience multiple chronic conditions simultaneously, compared to those with comorbidity, where one primary condition is accompanied by secondary disorders. Effective strategies include integrated care models and personalized treatment plans to reduce healthcare fragmentation, improve patient outcomes, and optimize resource allocation. Prioritizing multimorbidity in policy frameworks supports comprehensive care coordination and enhances management of complex health profiles within aging populations.
Future Directions in Research and Clinical Practice
Future research in multimorbidity should emphasize integrated care models that address multiple chronic conditions simultaneously, improving patient-centered outcomes and reducing healthcare fragmentation. Advancements in precision medicine and digital health tools hold promise for tailoring interventions based on complex disease interactions and individual patient profiles. Clinical practice must evolve to incorporate multidisciplinary teams and innovative decision-support systems that facilitate holistic management of multimorbidity beyond traditional comorbidity frameworks.
Multimorbidity Infographic
 libterm.com
libterm.com