Pericarditis is the inflammation of the pericardium, the thin sac surrounding the heart, often causing sharp chest pain and discomfort. Prompt diagnosis and treatment are essential to prevent complications such as cardiac tamponade or chronic constrictive pericarditis. Discover more about the symptoms, causes, and treatment options to protect your heart health in the rest of this article.
Table of Comparison
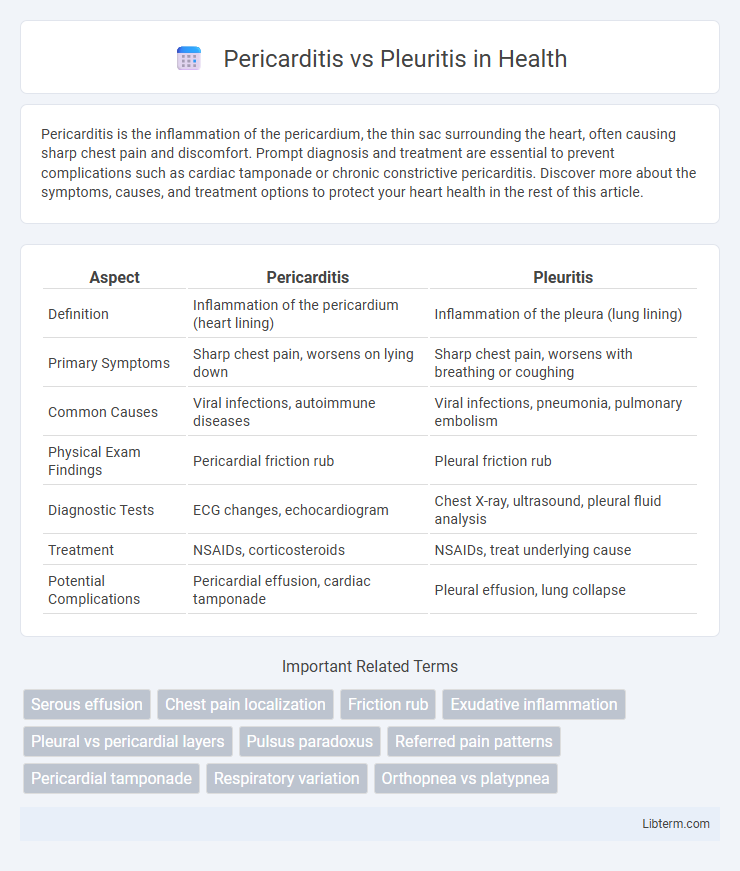
| Aspect | Pericarditis | Pleuritis |
|---|---|---|
| Definition | Inflammation of the pericardium (heart lining) | Inflammation of the pleura (lung lining) |
| Primary Symptoms | Sharp chest pain, worsens on lying down | Sharp chest pain, worsens with breathing or coughing |
| Common Causes | Viral infections, autoimmune diseases | Viral infections, pneumonia, pulmonary embolism |
| Physical Exam Findings | Pericardial friction rub | Pleural friction rub |
| Diagnostic Tests | ECG changes, echocardiogram | Chest X-ray, ultrasound, pleural fluid analysis |
| Treatment | NSAIDs, corticosteroids | NSAIDs, treat underlying cause |
| Potential Complications | Pericardial effusion, cardiac tamponade | Pleural effusion, lung collapse |
Introduction to Pericarditis and Pleuritis
Pericarditis is the inflammation of the pericardium, the double-layered sac surrounding the heart, often causing sharp chest pain and sometimes fluid accumulation between the layers. Pleuritis, also known as pleurisy, involves inflammation of the pleura, the membrane lining the lungs and chest cavity, characterized by sharp chest pain worsened by breathing or coughing. Both conditions mimic cardiac and pulmonary symptoms but differ in anatomical location and underlying causes, necessitating precise diagnostic approaches such as echocardiography for pericarditis and chest X-ray or ultrasound for pleuritis.
Definition and Overview
Pericarditis is the inflammation of the pericardium, the thin sac surrounding the heart, causing chest pain and potential fluid buildup. Pleuritis, also known as pleurisy, involves inflammation of the pleura, the membrane lining the lungs and chest cavity, leading to sharp chest pain during breathing. Both conditions share symptoms like chest pain but differ in anatomical location and underlying causes.
Causes and Risk Factors
Pericarditis commonly results from viral infections such as Coxsackievirus, autoimmune diseases like lupus, or post-myocardial infarction syndrome, while pleuritis is often caused by bacterial infections including pneumonia, pulmonary embolism, or autoimmune disorders like rheumatoid arthritis. Risk factors for pericarditis include recent viral illness, chest injury, and chronic kidney disease, whereas pleuritis risk factors encompass smoking, lung cancer, and heavy exposure to asbestos. Both conditions share autoimmune causes but differ substantially in infectious agents and environmental exposures influencing their occurrence.
Key Differences in Anatomy Involved
Pericarditis involves inflammation of the pericardium, the two-layered sac surrounding the heart, while pleuritis affects the pleura, the thin membranes lining the lungs and chest cavity. The pericardium primarily protects the heart and anchors it within the chest, whereas the pleura facilitates lung expansion and reduces friction during respiration. Distinct anatomical locations and functions make these inflammations clinically different, influencing symptom presentation such as chest pain and respiratory difficulty.
Signs and Symptoms Comparison
Pericarditis typically presents with sharp, pleuritic chest pain that worsens when lying down and improves when sitting up, accompanied by a pericardial friction rub heard on auscultation. Pleuritis, or pleurisy, causes localized chest pain that intensifies with deep breathing or coughing, often associated with a pleural rub and potentially accompanied by shortness of breath. Both conditions may present with fever and elevated inflammatory markers, but pericarditis often has positional pain and ECG changes, while pleuritis is more related to respiratory symptoms.
Diagnostic Approaches
Diagnostic approaches for pericarditis primarily involve echocardiography to detect pericardial effusion and electrocardiograms showing diffuse ST-segment elevation, while pleuritis diagnosis relies on chest X-rays and ultrasound to identify pleural effusion or thickening. Laboratory tests measuring inflammatory markers such as C-reactive protein and leukocyte count assist in both conditions but are not definitive for differentiation. Advanced imaging techniques like CT scans or MRI provide detailed visualization of pericardial and pleural structures, aiding in distinguishing pericarditis from pleuritis when clinical presentations overlap.
Treatment Options
Pericarditis treatment commonly involves nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and colchicine to reduce inflammation and pain. Pleuritis management also includes NSAIDs, with corticosteroids or antibiotics prescribed if an underlying infection or autoimmune condition is present. Both conditions may require drainage procedures in cases of significant fluid accumulation, highlighting the importance of accurate diagnosis for targeted therapy.
Complications and Prognosis
Pericarditis complications often include cardiac tamponade, constrictive pericarditis, and chronic pericardial effusion, which can impair heart function and require urgent intervention. Pleuritis complications may lead to pleural effusion, empyema, or fibrothorax, potentially causing respiratory distress and prolonged lung impairment. Prognosis for pericarditis generally depends on the underlying cause and timely treatment, with idiopathic cases often resolving fully, whereas pleuritis prognosis varies with etiology, severity, and effective management of associated infections or systemic diseases.
Prevention Strategies
Preventing pericarditis involves managing underlying infections such as viral or bacterial causes through timely treatment and maintaining good hygiene to reduce exposure. For pleuritis prevention, minimizing risk factors includes controlling respiratory infections, avoiding smoking, and managing chronic lung diseases like asthma or COPD. Vaccinations against influenza and pneumonia also play a significant role in lowering the incidence of both pericarditis and pleuritis.
When to Seek Medical Attention
Seek medical attention for pericarditis if experiencing sharp chest pain that worsens with deep breaths or lying down, accompanied by shortness of breath, fever, or fainting episodes. For pleuritis, urgent evaluation is necessary when chest pain intensifies during breathing, coughing, or sneezing, especially if it is accompanied by difficulty breathing, persistent cough, or fever. Prompt diagnosis and treatment are crucial to prevent complications such as cardiac tamponade in pericarditis or pleural effusion in pleuritis.
Pericarditis Infographic
 libterm.com
libterm.com