Anemia occurs when your blood lacks enough healthy red blood cells to carry adequate oxygen to the body's tissues, leading to fatigue and weakness. Causes range from nutritional deficiencies and chronic diseases to genetic conditions and blood loss. Discover effective treatments and prevention strategies by reading the rest of the article.
Table of Comparison
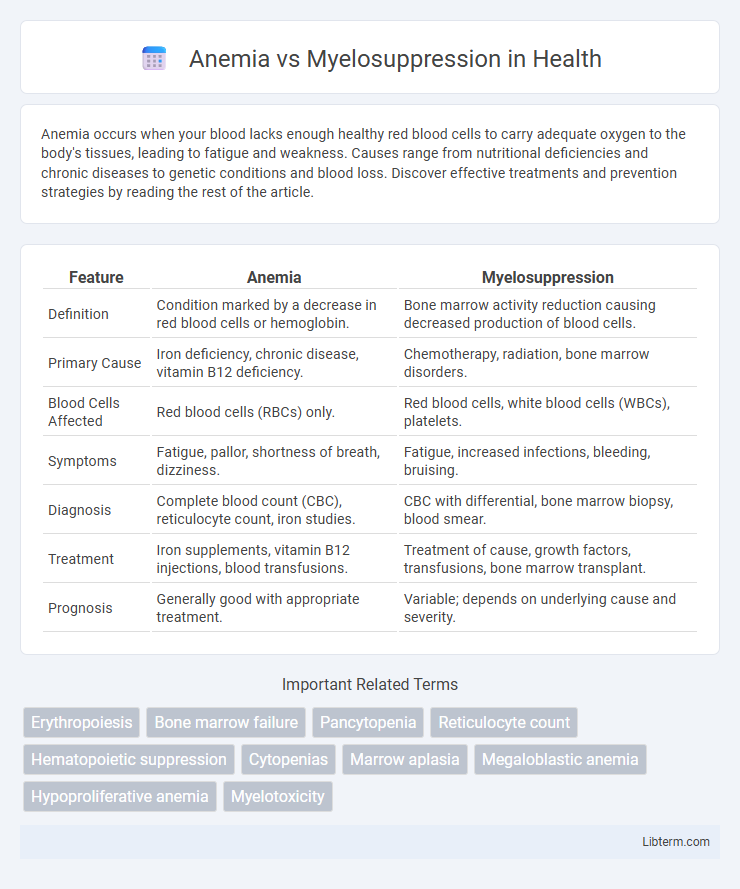
| Feature | Anemia | Myelosuppression |
|---|---|---|
| Definition | Condition marked by a decrease in red blood cells or hemoglobin. | Bone marrow activity reduction causing decreased production of blood cells. |
| Primary Cause | Iron deficiency, chronic disease, vitamin B12 deficiency. | Chemotherapy, radiation, bone marrow disorders. |
| Blood Cells Affected | Red blood cells (RBCs) only. | Red blood cells, white blood cells (WBCs), platelets. |
| Symptoms | Fatigue, pallor, shortness of breath, dizziness. | Fatigue, increased infections, bleeding, bruising. |
| Diagnosis | Complete blood count (CBC), reticulocyte count, iron studies. | CBC with differential, bone marrow biopsy, blood smear. |
| Treatment | Iron supplements, vitamin B12 injections, blood transfusions. | Treatment of cause, growth factors, transfusions, bone marrow transplant. |
| Prognosis | Generally good with appropriate treatment. | Variable; depends on underlying cause and severity. |
Understanding Anemia: Definition and Causes
Anemia is a condition characterized by a deficiency in the number or quality of red blood cells, leading to reduced oxygen transport in the body. Common causes include nutritional deficiencies (iron, vitamin B12, folate), chronic diseases, bone marrow disorders, and blood loss. Unlike myelosuppression, which directly impairs bone marrow function and affects multiple blood cell lines, anemia specifically impacts red blood cell production or lifespan.
Myelosuppression Explained: What It Means
Myelosuppression is a condition characterized by the decreased production of bone marrow cells, leading to reduced levels of red blood cells, white blood cells, and platelets. Unlike anemia, which specifically refers to a deficiency in red blood cells or hemoglobin, myelosuppression affects multiple blood cell lines, resulting in a broader spectrum of hematologic complications, including increased infection risk and bleeding tendencies. This condition is commonly caused by chemotherapy, radiation therapy, or certain medications that impair bone marrow function.
Key Differences Between Anemia and Myelosuppression
Anemia is a condition characterized by a deficiency in red blood cells or hemoglobin, leading to reduced oxygen transport in the body, whereas myelosuppression involves the decreased production of all blood cell types, including red blood cells, white blood cells, and platelets, due to bone marrow suppression. Anemia primarily results in fatigue, pallor, and shortness of breath, while myelosuppression increases the risk of infections, bleeding, and anemia symptoms. The causes differ significantly: anemia can arise from nutritional deficiencies, chronic diseases, or blood loss, whereas myelosuppression is commonly induced by chemotherapy, radiation therapy, or hematologic disorders.
Common Symptoms of Anemia vs Myelosuppression
Anemia and myelosuppression share symptoms such as fatigue and pallor, but anemia typically presents with shortness of breath and weakness due to reduced red blood cell count. Myelosuppression, a condition characterized by bone marrow failure, often causes increased infection risk and bleeding tendencies because of decreased white blood cells and platelets. Both conditions may exhibit overlapping signs yet differ significantly in underlying causes and hematologic impact.
Diagnostic Approaches: Anemia vs Myelosuppression
Diagnostic approaches for anemia primarily include complete blood count (CBC) to assess hemoglobin levels, hematocrit, and red blood cell indices, with further tests such as iron studies, vitamin B12, and folate levels to identify specific types. Myelosuppression diagnosis relies on bone marrow biopsy and aspiration to evaluate marrow cellularity and lineage-specific suppression, alongside peripheral blood counts showing pancytopenia or bicytopenia. Both conditions require differential diagnosis through clinical history, laboratory markers, and sometimes imaging to determine underlying causes and guide treatment.
Major Risk Factors Involved
Anemia primarily results from iron deficiency, chronic diseases, or vitamin B12 and folate shortages, which impair red blood cell production. Myelosuppression is predominantly caused by chemotherapy, radiation therapy, and bone marrow disorders that directly suppress bone marrow activity. Both conditions share risk factors such as chronic infections, autoimmune diseases, and certain medications that can disrupt normal hematopoiesis.
Treatment Options for Anemia and Myelosuppression
Treatment options for anemia primarily include iron supplementation, erythropoiesis-stimulating agents (ESAs), and blood transfusions depending on the anemia type and severity. Myelosuppression is managed by addressing the underlying cause, often involving dose adjustments of chemotherapeutic agents, administration of growth factors like granulocyte colony-stimulating factor (G-CSF), and supportive care to prevent infections. Both conditions require regular monitoring of blood counts and tailored therapeutic interventions to optimize patient outcomes.
Complications and Prognosis Comparison
Anemia primarily leads to complications such as fatigue, pallor, and increased cardiac workload, while myelosuppression often results in profound immunosuppression, increased infection risk, bleeding tendencies, and potential organ dysfunction. Prognosis for anemia varies depending on cause and treatment responsiveness, generally favorable with appropriate therapy, whereas myelosuppression carries a more guarded prognosis due to its association with bone marrow failure and increased morbidity from infections and hemorrhages. Effective management of myelosuppression requires prompt identification and supportive care to prevent life-threatening complications, contrasting with anemia where correction of the underlying etiology often ensures recovery.
Preventive Measures: Reducing Risk
Preventive measures for anemia include maintaining a diet rich in iron, vitamin B12, and folate, regular screening for at-risk populations, and managing chronic conditions effectively to reduce risk. Myelosuppression prevention focuses on monitoring blood cell counts during chemotherapy, administering growth factors like G-CSF, and avoiding exposure to toxins that can suppress bone marrow function. Early intervention and patient education on symptom recognition are crucial steps in minimizing complications from both conditions.
When to Seek Medical Attention
Seek medical attention for anemia if symptoms like persistent fatigue, shortness of breath, dizziness, or paleness worsen or fail to improve with dietary changes and iron supplementation. In cases of myelosuppression, urgent evaluation is necessary if signs of infection such as fever, chills, or unexplained bruising and bleeding occur, as these indicate severely compromised bone marrow function. Prompt diagnosis and treatment can prevent complications like severe anemia or life-threatening infections in both conditions.
Anemia Infographic
 libterm.com
libterm.com