Community-acquired infections occur outside of healthcare settings and often involve bacteria, viruses, or fungi that are prevalent in public environments. These infections can range from mild respiratory illnesses to more severe conditions requiring medical intervention. Explore the rest of the article to understand how to recognize, prevent, and treat community-acquired infections effectively.
Table of Comparison
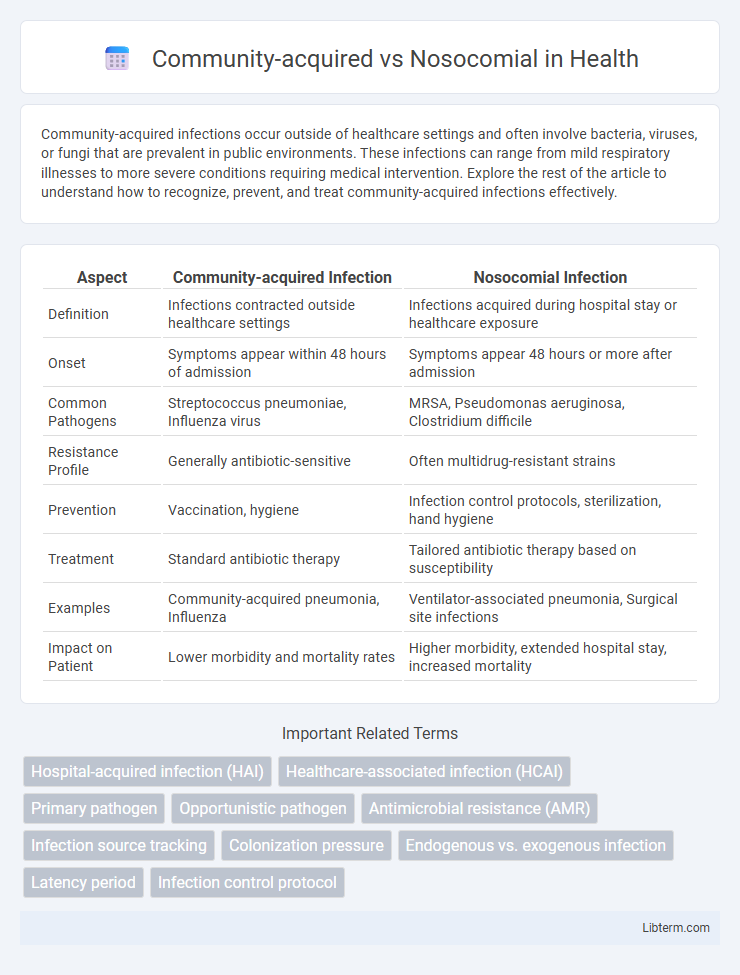
| Aspect | Community-acquired Infection | Nosocomial Infection |
|---|---|---|
| Definition | Infections contracted outside healthcare settings | Infections acquired during hospital stay or healthcare exposure |
| Onset | Symptoms appear within 48 hours of admission | Symptoms appear 48 hours or more after admission |
| Common Pathogens | Streptococcus pneumoniae, Influenza virus | MRSA, Pseudomonas aeruginosa, Clostridium difficile |
| Resistance Profile | Generally antibiotic-sensitive | Often multidrug-resistant strains |
| Prevention | Vaccination, hygiene | Infection control protocols, sterilization, hand hygiene |
| Treatment | Standard antibiotic therapy | Tailored antibiotic therapy based on susceptibility |
| Examples | Community-acquired pneumonia, Influenza | Ventilator-associated pneumonia, Surgical site infections |
| Impact on Patient | Lower morbidity and mortality rates | Higher morbidity, extended hospital stay, increased mortality |
Introduction to Community-acquired and Nosocomial Infections
Community-acquired infections occur outside healthcare settings and affect individuals with no recent hospital exposure, commonly caused by pathogens like Streptococcus pneumoniae and influenza viruses. Nosocomial infections, also known as healthcare-associated infections, develop during or after hospitalization, often involving resistant bacteria such as MRSA and Clostridium difficile. Understanding the distinct epidemiology and microbial profiles of these infections guides targeted prevention and treatment strategies.
Definitions: Community-acquired vs. Nosocomial Infections
Community-acquired infections originate outside healthcare settings and are present or incubating at the time of hospital admission, commonly caused by pathogens like Streptococcus pneumoniae. Nosocomial infections, also known as hospital-acquired infections, occur 48 hours or more after admission, often involving multidrug-resistant organisms such as MRSA and Pseudomonas aeruginosa. Accurate differentiation between community-acquired and nosocomial infections is essential for effective treatment strategies and infection control protocols.
Epidemiology and Prevalence
Community-acquired infections occur outside healthcare settings and typically affect individuals with no recent hospital exposure, exhibiting a higher prevalence due to widespread transmission in the general population. Nosocomial infections, also known as hospital-acquired infections, develop 48 hours or more after admission, with an increased incidence in intensive care units and among immunocompromised patients. Epidemiological data highlight that nosocomial infections contribute significantly to morbidity and mortality worldwide, accounting for approximately 7% of hospital patients affected in developed countries and up to 10% or more in developing regions.
Common Pathogens Involved
Community-acquired infections often involve pathogens such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus, which primarily affect otherwise healthy individuals outside healthcare settings. Nosocomial infections are frequently caused by multidrug-resistant organisms including Pseudomonas aeruginosa, Klebsiella pneumoniae, and Methicillin-resistant Staphylococcus aureus (MRSA), commonly acquired in hospitals or clinical environments. The distinction in common pathogens is critical for guiding empirical antibiotic therapy and infection control measures in clinical practice.
Risk Factors and Vulnerable Populations
Community-acquired infections often affect individuals with weakened immune systems, chronic illnesses, or those living in crowded conditions, increasing exposure risk. Nosocomial infections primarily impact hospitalized patients, especially those with invasive devices, prolonged hospital stays, or recent surgeries, due to exposure to resistant pathogens and compromised barriers. Elderly patients, neonates, and immunocompromised individuals represent vulnerable populations at high risk for both infection types due to inherent physiological and environmental factors.
Clinical Presentation and Diagnosis
Community-acquired infections typically present with acute symptoms such as fever, cough, and localized pain, often correlating with common pathogens like Streptococcus pneumoniae, while nosocomial infections manifest with more diverse and severe symptoms including persistent fever, sepsis, and organ dysfunction due to resistant organisms like MRSA and Pseudomonas aeruginosa. Diagnosis of community-acquired infections relies heavily on clinical history, physical examination, and routine cultures, whereas nosocomial infections require advanced diagnostic tools including molecular assays, imaging, and antimicrobial susceptibility testing to guide targeted therapy. Early identification through clinical scoring systems and biomarkers like procalcitonin improves differentiation and treatment outcomes between community-acquired and hospital-acquired infections.
Treatment Approaches and Protocols
Treatment approaches for community-acquired infections often involve empirical antibiotic therapy guided by local resistance patterns and common pathogens such as Streptococcus pneumoniae and Haemophilus influenzae. Nosocomial infections require targeted therapy based on hospital antibiograms, frequently addressing multidrug-resistant organisms like MRSA, Pseudomonas aeruginosa, and Clostridioides difficile. Protocols for nosocomial infections emphasize strict infection control measures, including isolation, antimicrobial stewardship, and routine surveillance to prevent transmission and ensure effective treatment outcomes.
Prevention and Infection Control Measures
Community-acquired infections require targeted prevention strategies such as vaccination, public awareness on hygiene, and timely diagnosis to reduce transmission outside healthcare settings. Nosocomial infections demand rigorous infection control measures including hand hygiene protocols, sterilization of medical equipment, and isolation of infected patients to prevent in-hospital spread. Effective surveillance systems and antimicrobial stewardship programs are critical in both environments to monitor infection trends and minimize resistance development.
Complications and Outcomes
Community-acquired infections often present with fewer complications due to earlier detection and treatment outside hospital settings, whereas nosocomial infections exhibit higher rates of multidrug resistance, leading to prolonged hospital stays and increased morbidity. Outcomes in nosocomial infections are typically worse, with elevated mortality rates linked to complications such as sepsis, organ failure, and delayed therapeutic response. Effective infection control and timely antimicrobial stewardship are critical to improving prognosis in nosocomial infection cases compared to community-acquired scenarios.
Future Trends and Research Directions
Emerging research in infectious diseases highlights the growing importance of genomic surveillance and rapid diagnostic tools to distinguish between community-acquired and nosocomial infections, enabling targeted antimicrobial therapies. Advances in machine learning and big data analytics are shaping predictive models for infection outbreaks, improving hospital infection control protocols and public health strategies. Future trends emphasize personalized medicine approaches and the integration of real-time electronic health records to monitor pathogen resistance patterns and transmission dynamics effectively.
Community-acquired Infographic
 libterm.com
libterm.com