Stenosis is a medical condition characterized by the abnormal narrowing of blood vessels or other tubular organs, which restricts blood flow or passage of fluids. This narrowing can cause symptoms such as pain, numbness, or organ dysfunction depending on the affected area. Discover how stenosis impacts your health and the available treatment options in the full article.
Table of Comparison
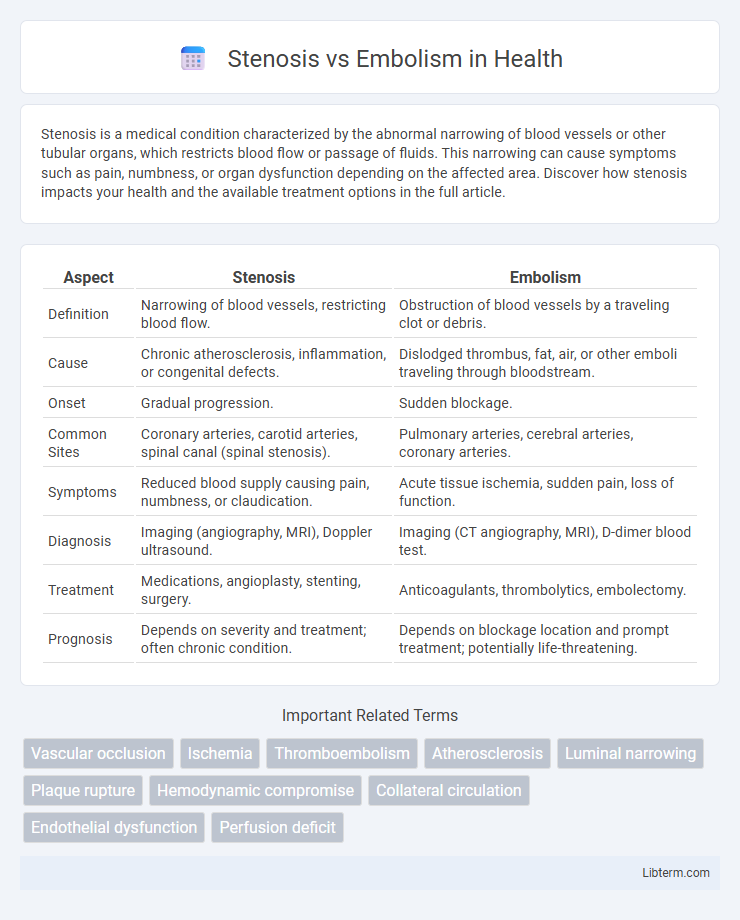
| Aspect | Stenosis | Embolism |
|---|---|---|
| Definition | Narrowing of blood vessels, restricting blood flow. | Obstruction of blood vessels by a traveling clot or debris. |
| Cause | Chronic atherosclerosis, inflammation, or congenital defects. | Dislodged thrombus, fat, air, or other emboli traveling through bloodstream. |
| Onset | Gradual progression. | Sudden blockage. |
| Common Sites | Coronary arteries, carotid arteries, spinal canal (spinal stenosis). | Pulmonary arteries, cerebral arteries, coronary arteries. |
| Symptoms | Reduced blood supply causing pain, numbness, or claudication. | Acute tissue ischemia, sudden pain, loss of function. |
| Diagnosis | Imaging (angiography, MRI), Doppler ultrasound. | Imaging (CT angiography, MRI), D-dimer blood test. |
| Treatment | Medications, angioplasty, stenting, surgery. | Anticoagulants, thrombolytics, embolectomy. |
| Prognosis | Depends on severity and treatment; often chronic condition. | Depends on blockage location and prompt treatment; potentially life-threatening. |
Understanding Stenosis and Embolism: Definitions
Stenosis refers to the abnormal narrowing of blood vessels or other tubular structures, reducing blood flow and causing tissue ischemia. Embolism involves the sudden blockage of a blood vessel by a floating clot, air bubble, or other foreign material that obstructs circulation. Understanding the distinct definitions of stenosis and embolism is crucial for accurate diagnosis and targeted treatment in vascular and cardiovascular medicine.
Key Differences Between Stenosis and Embolism
Stenosis refers to the narrowing of blood vessels or other tubular structures, often caused by atherosclerosis or inflammation, which reduces blood flow over time. Embolism involves the sudden blockage of a blood vessel by a foreign substance such as a blood clot, fat globule, or air bubble that travels through the bloodstream. The key difference lies in stenosis being a gradual constriction, whereas embolism is an acute obstruction, leading to different clinical presentations and treatment approaches.
Causes of Stenosis
Stenosis primarily results from atherosclerosis, where plaque buildup narrows blood vessels, reducing blood flow and causing ischemia. Other causes include congenital abnormalities, inflammation, or scarring from injury or infection that thickens or stiffens vessel walls. These factors lead to vessel lumen constriction, distinguishing stenosis from embolism, which is caused by emboli blocking blood vessels.
Causes of Embolism
Embolism is primarily caused by thrombi originating from deep vein thrombosis, atrial fibrillation, or atherosclerotic plaque rupture releasing debris into the bloodstream. Other causes include fat emboli from long bone fractures, air embolism during surgical procedures, and septic emboli from infective endocarditis. Unlike stenosis, which involves vessel narrowing due to plaque buildup or fibrosis, embolism abruptly obstructs blood flow through detached intravascular material.
Symptoms of Stenosis vs Embolism
Symptoms of stenosis typically include localized pain, numbness, and weakness due to reduced blood flow caused by vessel narrowing, often leading to gradual onset of symptoms. Embolism symptoms present suddenly and may involve intense pain, loss of function, or tissue ischemia, depending on the affected organ, such as sudden limb coldness or neurological deficits in stroke. Differentiating symptoms is crucial for timely diagnosis and treatment, as stenosis reflects chronic vessel constriction while embolism denotes acute arterial blockage.
Diagnostic Approaches for Stenosis and Embolism
Diagnostic approaches for stenosis typically involve imaging techniques such as Doppler ultrasound, magnetic resonance angiography (MRA), and computed tomography angiography (CTA) to assess vessel narrowing and blood flow disruption. Embolism diagnosis often relies on prompt identification using transesophageal echocardiography (TEE), CT pulmonary angiography (CTPA), and ventilation-perfusion (V/Q) scans to detect emboli in the pulmonary arteries or systemic circulation. Biomarkers like D-dimer tests aid in embolism evaluation but are less relevant for stenosis detection.
Treatment Options for Stenosis
Treatment options for stenosis primarily include angioplasty and stenting to restore adequate blood flow by widening the narrowed arteries. In cases where minimally invasive procedures are insufficient, surgical interventions like endarterectomy or bypass surgery may be necessary. Medical management often involves antiplatelet agents, statins, and lifestyle modifications to prevent progression and reduce cardiovascular risk.
Treatment Options for Embolism
Treatment options for embolism primarily focus on restoring blood flow and preventing further clot formation. Anticoagulant medications such as heparin and warfarin are commonly administered to inhibit clot growth, while thrombolytic therapy using agents like tissue plasminogen activator (tPA) helps dissolve existing emboli. In severe cases, surgical interventions including embolectomy or catheter-directed thrombectomy may be necessary to remove the obstruction and reduce tissue damage.
Complications Associated with Stenosis and Embolism
Stenosis often leads to complications such as reduced blood flow, which can cause ischemia, tissue damage, and organ dysfunction, particularly in the heart and brain. Embolism can result in sudden blockage of blood vessels, causing acute ischemic events like stroke, pulmonary embolism, or limb ischemia. Both conditions increase the risk of severe complications including infarction, organ failure, and chronic morbidity if untreated.
Preventive Strategies for Stenosis and Embolism
Preventive strategies for stenosis emphasize managing risk factors such as hypertension, hyperlipidemia, and diabetes through lifestyle changes and medication adherence to reduce arterial plaque buildup. Embolism prevention centers on anticoagulation therapy in patients with atrial fibrillation or deep vein thrombosis, combined with regular monitoring to avoid thrombus formation and subsequent vessel occlusion. Both conditions benefit from routine vascular assessments and timely intervention to minimize ischemic complications.
Stenosis Infographic
 libterm.com
libterm.com