Thalassemia is a hereditary blood disorder characterized by the body's inability to produce adequate hemoglobin, leading to anemia and fatigue. Effective management includes regular blood transfusions, iron chelation therapy, and genetic counseling to reduce complications. Discover how thalassemia impacts your health and the latest treatments by reading the full article.
Table of Comparison
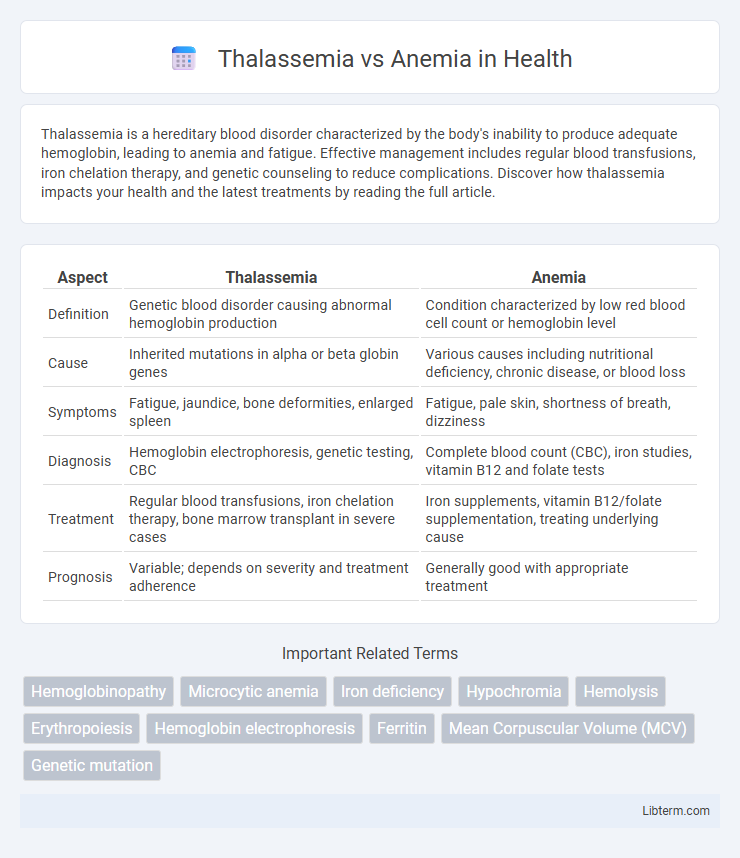
| Aspect | Thalassemia | Anemia |
|---|---|---|
| Definition | Genetic blood disorder causing abnormal hemoglobin production | Condition characterized by low red blood cell count or hemoglobin level |
| Cause | Inherited mutations in alpha or beta globin genes | Various causes including nutritional deficiency, chronic disease, or blood loss |
| Symptoms | Fatigue, jaundice, bone deformities, enlarged spleen | Fatigue, pale skin, shortness of breath, dizziness |
| Diagnosis | Hemoglobin electrophoresis, genetic testing, CBC | Complete blood count (CBC), iron studies, vitamin B12 and folate tests |
| Treatment | Regular blood transfusions, iron chelation therapy, bone marrow transplant in severe cases | Iron supplements, vitamin B12/folate supplementation, treating underlying cause |
| Prognosis | Variable; depends on severity and treatment adherence | Generally good with appropriate treatment |
Understanding Thalassemia and Anemia
Thalassemia and anemia both involve deficiencies in red blood cells or hemoglobin but differ in their underlying causes and genetic implications. Thalassemia is a hereditary blood disorder characterized by reduced or absent production of hemoglobin chains, leading to chronic anemia and requiring lifelong management. Anemia, on the other hand, can result from various factors such as iron deficiency, vitamin B12 deficiency, or chronic disease, and it is typically treatable depending on the cause.
Causes of Thalassemia vs Anemia
Thalassemia is caused by genetic mutations affecting hemoglobin production, leading to defective or insufficient hemoglobin chains. Anemia results from various factors including nutritional deficiencies (iron, vitamin B12, folate), chronic diseases, blood loss, or bone marrow disorders. Unlike anemia's diverse causes, thalassemia specifically arises from inherited abnormalities in globin gene synthesis.
Genetic Factors in Thalassemia and Anemia
Thalassemia is a genetic blood disorder caused by mutations in the HBB or HBA genes leading to abnormal hemoglobin production. Anemia, while often caused by nutritional deficiencies or chronic diseases, can also have genetic origins such as hereditary spherocytosis or G6PD deficiency. Genetic factors in thalassemia directly impair hemoglobin synthesis, whereas genetic anemia often involves defects in red blood cell structure or enzyme function.
Key Symptoms: Thalassemia vs Anemia
Thalassemia primarily presents with symptoms such as severe fatigue, jaundice, dark urine, and bone deformities due to ineffective red blood cell production. Anemia commonly manifests as weakness, pallor, shortness of breath, and dizziness caused by reduced hemoglobin or red blood cell count. While both conditions share fatigue and pallor, thalassemia's distinct signs include skeletal abnormalities and pronounced jaundice, distinguishing it from general anemia symptoms.
Diagnosis: Testing Methods and Criteria
Diagnosis of thalassemia primarily involves complete blood count (CBC) revealing microcytic hypochromic anemia with normal or elevated red blood cell count, followed by hemoglobin electrophoresis to detect abnormal hemoglobin variants characteristic of alpha or beta thalassemia. Anemia diagnosis requires identifying underlying causes through CBC indicating decreased hemoglobin levels and mean corpuscular volume (MCV), with further tests such as serum ferritin for iron-deficiency anemia or bone marrow biopsy for unexplained cases. Genetic testing and DNA analysis confirm thalassemia mutations, differentiating it from iron-deficiency anemia, which lacks such mutations and shows distinct biochemical markers.
Differences in Treatment Approaches
Treatment approaches for thalassemia often include regular blood transfusions and iron chelation therapy to manage iron overload, while anemia treatment depends on the underlying cause, such as iron supplements for iron-deficiency anemia or vitamin B12 injections for pernicious anemia. Thalassemia may also require bone marrow or stem cell transplantation as a potential curative option, whereas anemia rarely involves such advanced interventions. The management intensity and complexity in thalassemia are significantly higher compared to most common forms of anemia.
Complications and Risks: Thalassemia vs Anemia
Thalassemia poses higher risks of severe complications including iron overload, bone deformities, and spleen enlargement due to ineffective hemoglobin production, whereas anemia generally leads to fatigue, weakness, and impaired oxygen delivery with fewer long-term organ damages. Patients with thalassemia often require frequent blood transfusions, increasing the risk of infections and cardiac issues, while anemia complications largely depend on its underlying cause such as nutritional deficiencies or chronic diseases. Managing thalassemia demands specialized treatments like chelation therapy to prevent iron toxicity, contrasting with anemia's typically simpler interventions focused on addressing its root causes.
Prevention and Genetic Counseling
Thalassemia prevention involves genetic counseling to identify carriers and assess the risk of passing the disorder to offspring, enabling informed family planning decisions. Anemia prevention focuses on addressing nutritional deficiencies, particularly iron, vitamin B12, and folate intake, through diet or supplementation. Genetic counseling is crucial for thalassemia due to its hereditary nature, while anemia often requires lifestyle and medical interventions tailored to its specific causes.
Living with Thalassemia and Anemia
Living with Thalassemia requires regular blood transfusions and iron chelation therapy to manage chronic anemia and prevent complications like organ damage. Individuals with anemia benefit from dietary changes, iron supplements, or treatment of underlying causes to improve energy levels and quality of life. Both conditions necessitate ongoing medical care and lifestyle adjustments to maintain optimal health and reduce symptoms.
Prognosis and Long-term Outlook
Thalassemia prognosis varies by type, with beta-thalassemia major requiring lifelong blood transfusions and iron chelation therapy to prevent severe complications, while thalassemia minor often presents with a normal lifespan and minimal symptoms. Anemia's long-term outlook depends on its cause; nutritional anemias resolve well with proper supplementation, whereas chronic disease-related or untreated anemia may lead to organ damage or reduced quality of life. Both conditions necessitate tailored management strategies to optimize patient outcomes and mitigate potential complications.
Thalassemia Infographic
 libterm.com
libterm.com