Asystole, commonly known as flatline, is a life-threatening cardiac arrest condition characterized by the absence of electrical activity in the heart, leading to a cessation of heartbeat and circulation. Immediate medical intervention, including CPR and advanced cardiac life support, is crucial to improve survival chances. Explore the article to understand the causes, symptoms, and emergency treatment steps for asystole.
Table of Comparison
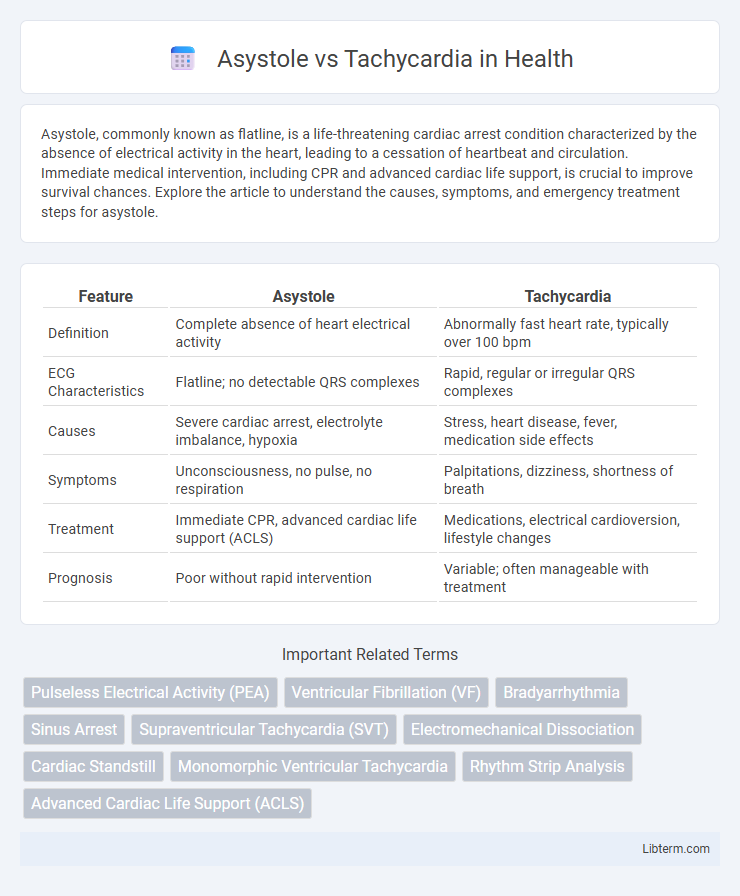
| Feature | Asystole | Tachycardia |
|---|---|---|
| Definition | Complete absence of heart electrical activity | Abnormally fast heart rate, typically over 100 bpm |
| ECG Characteristics | Flatline; no detectable QRS complexes | Rapid, regular or irregular QRS complexes |
| Causes | Severe cardiac arrest, electrolyte imbalance, hypoxia | Stress, heart disease, fever, medication side effects |
| Symptoms | Unconsciousness, no pulse, no respiration | Palpitations, dizziness, shortness of breath |
| Treatment | Immediate CPR, advanced cardiac life support (ACLS) | Medications, electrical cardioversion, lifestyle changes |
| Prognosis | Poor without rapid intervention | Variable; often manageable with treatment |
Introduction to Asystole and Tachycardia
Asystole is a life-threatening cardiac condition characterized by the complete absence of electrical activity in the heart, leading to no contraction and cessation of blood circulation. Tachycardia refers to an abnormally fast heart rate, typically exceeding 100 beats per minute, which can disrupt normal cardiac function and oxygen delivery. Both conditions require prompt medical evaluation and intervention due to their impact on hemodynamic stability and potential to cause cardiac arrest.
Definition and Overview
Asystole is a life-threatening cardiac condition characterized by the complete absence of electrical activity in the heart, leading to no heartbeat and cessation of blood circulation. Tachycardia is defined by an abnormally fast heart rate, typically exceeding 100 beats per minute in adults, which can reduce cardiac efficiency and compromise oxygen delivery to tissues. Both conditions require prompt medical evaluation and intervention to prevent severe outcomes such as cardiac arrest or organ damage.
Causes of Asystole
Asystole, characterized by a complete absence of ventricular electrical activity, primarily results from severe myocardial ischemia, prolonged hypoxia, or advanced cardiac arrest scenarios. Unlike tachycardia, which involves abnormally rapid heart rhythms often triggered by electrolyte imbalances, stress, or structural heart disease, asystole indicates a critical failure of the heart's electrical conduction system. Immediate identification of underlying causes such as hypoxia, acidosis, or extensive myocardial infarction is vital for effective resuscitation efforts in asystolic patients.
Causes of Tachycardia
Tachycardia, characterized by an abnormally fast heart rate exceeding 100 beats per minute, often results from causes such as stress, fever, anemia, hyperthyroidism, and excessive caffeine or stimulant intake. Other factors include heart-related conditions like arrhythmias, myocardial infarction, and heart failure, as well as electrolyte imbalances and drug side effects. Unlike asystole, which is a state of cardiac arrest with no electrical activity, tachycardia reflects an active but potentially dysfunctional cardiac rhythm requiring prompt evaluation and management.
Clinical Presentation and Symptoms
Asystole presents clinically as sudden loss of consciousness and absence of palpable pulse, reflecting complete cardiac arrest with no electrical activity in the heart. Tachycardia is characterized by rapid heart rates exceeding 100 beats per minute, often causing palpitations, dizziness, chest pain, and shortness of breath. While asystole requires immediate resuscitation interventions, tachycardia symptoms vary from asymptomatic to severe, depending on underlying causes and rate severity.
ECG Findings: Asystole vs Tachycardia
Asystole ECG shows a flatline or absent electrical activity, indicating no ventricular contractions and no pulse, whereas tachycardia is characterized by a rapid heart rate exceeding 100 beats per minute, presenting with closely spaced QRS complexes and often narrow or wide QRS morphology depending on the origin. Tachycardia may display regular or irregular rhythm, with P waves present, absent, or abnormal based on the type (e.g., supraventricular or ventricular tachycardia). The distinction on ECG is critical for diagnosis and treatment, as asystole requires immediate resuscitation efforts, while tachycardia management varies based on the underlying cause and hemodynamic stability.
Emergency Management Strategies
Asystole requires immediate initiation of cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) protocols, including administration of epinephrine and assessment for reversible causes of cardiac arrest. Tachycardia management depends on the type and stability of the patient, with unstable patients needing synchronized cardioversion, while stable patients may benefit from vagal maneuvers, rate-controlling medications like beta-blockers or calcium channel blockers, and antiarrhythmic drugs. Rapid diagnosis and tailored interventions are critical to improving outcomes in both asystole and tachycardia emergencies.
Prognosis and Outcomes
Asystole, characterized by the complete absence of ventricular electrical activity, typically results in poor prognosis with survival rates under 5% without immediate intervention due to irreversible cardiac arrest. Tachycardia, defined by abnormally fast heart rates above 100 beats per minute, presents variable outcomes depending on the underlying cause, with supraventricular tachycardia often manageable and ventricular tachycardia posing higher risks of sudden cardiac death. Early defibrillation and advanced cardiac life support improve outcomes in tachyarrhythmias, whereas asystole requires prompt CPR and identification of reversible causes to enhance survival chances.
Prevention and Risk Reduction
Preventing asystole involves managing underlying cardiac conditions, maintaining electrolyte balance, and avoiding drug toxicities that can lead to cardiac arrest. Risk reduction for tachycardia centers on controlling hypertension, reducing stress, avoiding stimulants like caffeine and nicotine, and treating arrhythmias with appropriate medications or procedures. Regular cardiovascular check-ups and lifestyle modifications, including a heart-healthy diet and consistent exercise, play critical roles in minimizing the chances of both conditions.
Key Differences: Asystole vs Tachycardia
Asystole is characterized by the complete absence of cardiac electrical activity, resulting in a flatline on an ECG and no heartbeat, whereas tachycardia involves an abnormally fast heart rate, typically above 100 beats per minute. The primary distinction lies in electrical activity: asystole shows no electrical impulses, while tachycardia features rapid but organized electrical signals causing accelerated heart contractions. Clinically, asystole is a non-perfusing rhythm requiring immediate resuscitation, whereas tachycardia may be either benign or symptomatic depending on underlying causes and heart function.
Asystole Infographic
 libterm.com
libterm.com