Hypokalemia occurs when blood potassium levels drop below normal, disrupting muscle function and leading to symptoms like weakness, cramps, and irregular heart rhythms. Treatment focuses on restoring potassium balance through diet or supplements while addressing underlying causes such as medication side effects or medical conditions. Explore the rest of the article to understand how you can recognize, manage, and prevent hypokalemia effectively.
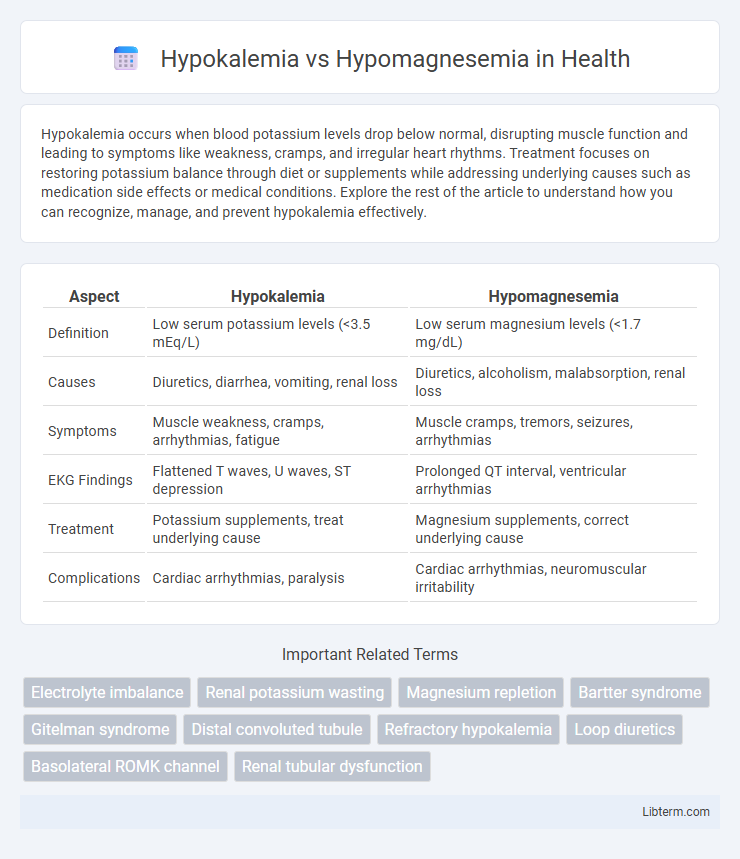
Table of Comparison
| Aspect | Hypokalemia | Hypomagnesemia |
|---|---|---|
| Definition | Low serum potassium levels (<3.5 mEq/L) | Low serum magnesium levels (<1.7 mg/dL) |
| Causes | Diuretics, diarrhea, vomiting, renal loss | Diuretics, alcoholism, malabsorption, renal loss |
| Symptoms | Muscle weakness, cramps, arrhythmias, fatigue | Muscle cramps, tremors, seizures, arrhythmias |
| EKG Findings | Flattened T waves, U waves, ST depression | Prolonged QT interval, ventricular arrhythmias |
| Treatment | Potassium supplements, treat underlying cause | Magnesium supplements, correct underlying cause |
| Complications | Cardiac arrhythmias, paralysis | Cardiac arrhythmias, neuromuscular irritability |
Understanding Hypokalemia and Hypomagnesemia
Hypokalemia is characterized by low serum potassium levels below 3.5 mEq/L, causing muscle weakness, cardiac arrhythmias, and fatigue due to impaired cellular function. Hypomagnesemia involves decreased serum magnesium below 1.7 mg/dL, disrupting neuromuscular transmission, leading to muscle cramps, tetany, and refractory hypokalemia. Both conditions often coexist because magnesium deficiency impairs renal potassium retention, making simultaneous correction essential for effective treatment.
Etiology: Causes of Hypokalemia vs Hypomagnesemia
Hypokalemia is commonly caused by excessive gastrointestinal losses such as vomiting or diarrhea, diuretic use, and inadequate potassium intake, whereas hypomagnesemia frequently results from chronic alcoholism, malabsorption syndromes, and prolonged use of medications like proton pump inhibitors or diuretics. Renal potassium wasting, seen in conditions like hyperaldosteronism, contributes significantly to hypokalemia, while hypomagnesemia often arises from impaired intestinal absorption or increased renal excretion of magnesium. Identifying the distinct etiologies of hypokalemia and hypomagnesemia is critical for accurate diagnosis and targeted treatment strategies.
Pathophysiological Differences
Hypokalemia involves a decrease in serum potassium levels primarily due to increased renal excretion, intracellular shifting, or inadequate intake, leading to impaired membrane potential and muscle weakness. In contrast, hypomagnesemia results from magnesium depletion through gastrointestinal losses or renal wasting, disrupting enzymatic processes and ion transport affecting neuromuscular excitability. The pathophysiological distinction lies in hypokalemia's direct impact on potassium channels and cellular excitability, whereas hypomagnesemia primarily affects magnesium-dependent enzymatic reactions and modulation of potassium and calcium channels.
Clinical Manifestations: Signs and Symptoms
Hypokalemia often presents with muscle weakness, cramps, fatigue, and cardiac arrhythmias such as premature ventricular contractions or tachycardia, while hypomagnesemia may cause neuromuscular irritability including tremors, tetany, and seizures along with cardiac arrhythmias like torsades de pointes. Both conditions can manifest with symptoms of electrolyte imbalance, but hypomagnesemia frequently leads to more severe neurological signs and refractory hypokalemia. Recognizing these clinical manifestations is crucial for differential diagnosis and effective management in patients with electrolyte disorders.
Diagnostic Approaches and Laboratory Findings
Hypokalemia is identified through serum potassium levels below 3.5 mEq/L, often accompanied by electrocardiogram changes such as flattened T waves and U waves, whereas hypomagnesemia presents with serum magnesium levels under 1.7 mg/dL, frequently causing refractory hypokalemia due to magnesium's role in potassium homeostasis. Diagnostic approaches involve comprehensive electrolyte panels, with hypomagnesemia requiring measurement of ionized magnesium or 24-hour urine magnesium to differentiate between renal and gastrointestinal losses. Laboratory findings also include assessment of urinary potassium excretion; low in hypokalemia due to inadequate intake or shift, but high in magnesium deficiency indicating renal potassium wasting secondary to magnesium depletion.
Electrolyte Interactions and Overlap
Hypokalemia and hypomagnesemia frequently coexist due to magnesium's critical role in potassium homeostasis, where magnesium deficiency impairs the Na+/K+-ATPase pump, leading to intracellular potassium loss. Both electrolyte disturbances disrupt cardiac and neuromuscular function, often exacerbating each other and complicating clinical management. Correcting hypomagnesemia is essential to effectively restore potassium levels and stabilize cellular excitability.
Risk Factors and Patient Populations
Hypokalemia risk factors include diuretic use, vomiting, diarrhea, and conditions like hyperaldosteronism, frequently affecting patients with heart failure or hypertension. Hypomagnesemia commonly arises from chronic alcoholism, malabsorption syndromes, or prolonged proton pump inhibitor use, predominantly impacting individuals with malnutrition or gastrointestinal disorders. Both electrolyte disturbances are prevalent in critically ill patients, with increased susceptibility in the elderly due to comorbidities and polypharmacy.
Treatment Strategies and Management
Treatment strategies for hypokalemia primarily involve potassium supplementation through oral or intravenous routes to restore normal serum potassium levels, alongside addressing underlying causes such as diuretic use or gastrointestinal losses. Management of hypomagnesemia centers on magnesium replacement, typically via oral magnesium oxide or intravenous magnesium sulfate in severe cases, while correcting concurrent electrolyte imbalances like hypokalemia to ensure effective normalization. Both conditions require continuous monitoring of electrolyte levels and cardiac function to prevent complications such as arrhythmias and muscular weakness during the correction process.
Complications and Prognosis
Hypokalemia can cause potentially life-threatening cardiac arrhythmias and muscular weakness, increasing the risk of respiratory failure and prolonged hospital stays. Hypomagnesemia often leads to refractory hypokalemia, seizures, and neuromuscular irritability, complicating electrolyte management and worsening patient outcomes. Both conditions require prompt correction to prevent severe complications and improve long-term prognosis, with untreated cases linked to increased morbidity and mortality.
Prevention and Monitoring Recommendations
Preventing hypokalemia and hypomagnesemia requires regular monitoring of serum electrolyte levels, particularly in high-risk populations such as patients on diuretics, those with gastrointestinal losses, or individuals with chronic kidney disease. Ensuring adequate dietary intake of potassium-rich foods like bananas and spinach, alongside magnesium sources such as nuts and whole grains, is essential for maintaining electrolyte balance. Routine assessment through blood tests and electrocardiograms helps detect early electrolyte disturbances, enabling timely intervention to prevent complications like cardiac arrhythmias.
Hypokalemia Infographic
 libterm.com
libterm.com