Bioequivalence ensures that a generic drug releases its active ingredient into the bloodstream at the same rate and extent as the brand-name drug, guaranteeing similar therapeutic effects. Generic equivalence confirms that the generic product meets all regulatory standards to be interchangeable with the original medication, ensuring safety and efficacy. Discover how understanding these concepts can affect Your medication choices by reading the rest of the article.
Table of Comparison
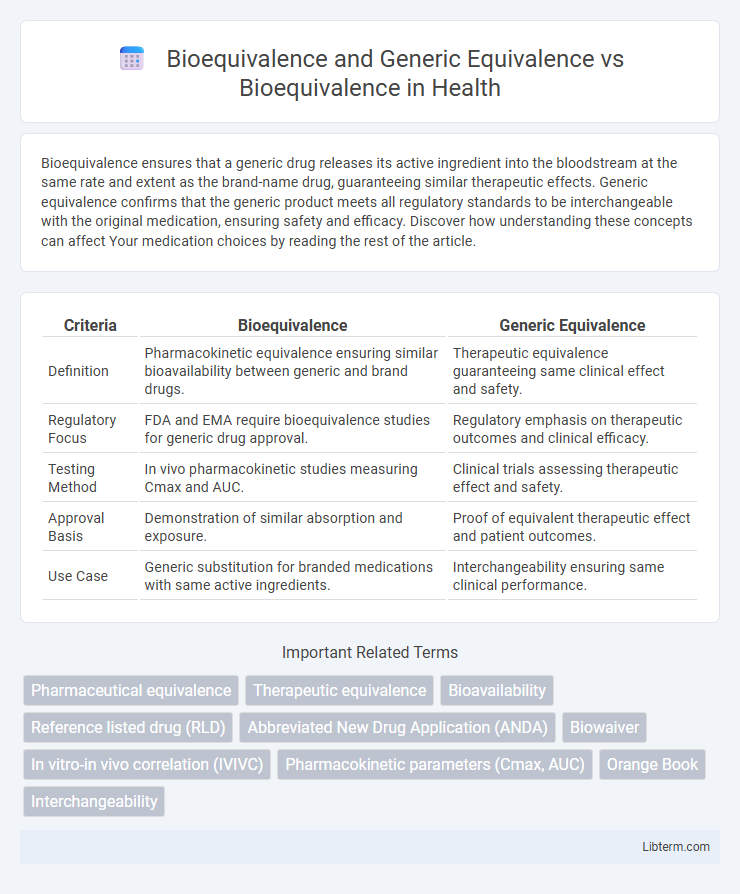
| Criteria | Bioequivalence | Generic Equivalence |
|---|---|---|
| Definition | Pharmacokinetic equivalence ensuring similar bioavailability between generic and brand drugs. | Therapeutic equivalence guaranteeing same clinical effect and safety. |
| Regulatory Focus | FDA and EMA require bioequivalence studies for generic drug approval. | Regulatory emphasis on therapeutic outcomes and clinical efficacy. |
| Testing Method | In vivo pharmacokinetic studies measuring Cmax and AUC. | Clinical trials assessing therapeutic effect and safety. |
| Approval Basis | Demonstration of similar absorption and exposure. | Proof of equivalent therapeutic effect and patient outcomes. |
| Use Case | Generic substitution for branded medications with same active ingredients. | Interchangeability ensuring same clinical performance. |
Understanding Bioequivalence: Definition and Importance
Bioequivalence refers to the absence of a significant difference in the rate and extent of absorption of the active ingredient between two pharmaceutical products under similar conditions. It is crucial for ensuring that a generic drug performs the same as its brand-name counterpart in terms of safety, efficacy, and therapeutic effect. Establishing bioequivalence supports regulatory approval and promotes patient confidence by confirming that the generic product can be substituted interchangeably with the original drug.
The Science Behind Bioequivalence Studies
Bioequivalence studies scientifically compare the pharmacokinetic properties--such as absorption rate and plasma concentration-time profiles--of a generic drug to its reference listed drug to ensure therapeutic equivalence. These studies measure parameters like Cmax (maximum concentration), Tmax (time to reach Cmax), and AUC (area under the curve) to confirm comparable bioavailability between formulations. Unlike generic equivalence, which often relies on pharmaceutical equivalence and dosage form similarity, bioequivalence requires rigorous in vivo testing to demonstrate that the generic performs identically in the body.
Regulatory Framework for Bioequivalence Assessment
Regulatory frameworks for bioequivalence assessment mandate rigorous pharmacokinetic studies to ensure generic drugs exhibit comparable bioavailability to their reference products, ensuring therapeutic equivalence. Agencies such as the FDA and EMA require generic equivalents to meet strict criteria on parameters like Cmax and AUC within accepted confidence intervals, typically 80-125%. These standardized evaluation protocols ensure that both bioequivalence and generic equivalence uphold safety, efficacy, and quality standards crucial for market authorization.
Key Parameters Measured in Bioequivalence
Key parameters measured in bioequivalence include the rate and extent of drug absorption, typically quantified by Cmax (maximum concentration) and AUC (area under the curve). These metrics assess whether the generic product releases the active ingredient into the bloodstream at a comparable rate and extent as the reference drug. In contrast to generic equivalence, which focuses mainly on pharmaceutical formulation similarity, bioequivalence rigorously ensures therapeutic equivalence through pharmacokinetic data.
Generic Equivalence vs. Bioequivalence: Clarifying the Terms
Generic equivalence refers to drugs that contain the same active ingredients, dosage form, strength, and route of administration as the brand-name product but may not have demonstrated bioequivalence through pharmacokinetic studies. Bioequivalence requires that the generic drug shows no significant difference in the rate and extent of absorption compared to the reference drug, ensuring therapeutic equivalence. Clarifying these terms is crucial for healthcare providers and patients to understand that generic equivalence alone does not guarantee the same clinical effectiveness as bioequivalence-confirmed products.
Steps in Establishing Generic Drug Equivalence
Establishing generic drug equivalence involves rigorous bioequivalence studies to ensure the generic product delivers the same therapeutic effect as the branded drug. Key steps include selecting appropriate study design, conducting pharmacokinetic assessments such as measuring Cmax and AUC, and statistically analyzing data within FDA-specified equivalence margins (80-125%). Regulatory approval depends on demonstrating comparable bioavailability, safety, and efficacy without clinically meaningful differences.
Clinical and Statistical Criteria for Bioequivalence
Clinical and statistical criteria for bioequivalence focus on ensuring that generic drugs exhibit no significant difference in the rate and extent of absorption compared to their branded counterparts. Key parameters include the 90% confidence intervals for the ratios of pharmacokinetic measures such as Cmax (peak concentration) and AUC (area under the curve), which must typically fall within the 80-125% range. Unlike generic equivalence, which primarily considers pharmaceutical and therapeutic equivalence, bioequivalence requires rigorous clinical trials and statistical analysis to confirm comparable efficacy and safety profiles.
Common Challenges in Demonstrating Bioequivalence
Demonstrating bioequivalence faces common challenges such as variability in drug absorption rates, differences in formulation excipients, and inter-subject pharmacokinetic variability that complicate consistent measurement. Regulatory criteria require that generic drugs show comparable bioavailability to the reference product within predefined statistical limits, often demanding rigorous in vivo studies under controlled conditions. Complexities arise in assessing narrow therapeutic index drugs and highly variable drugs, requiring advanced study designs and thorough statistical analysis to ensure therapeutic equivalence.
Impact of Bioequivalence on Drug Approval and Patient Access
Bioequivalence plays a critical role in drug approval by demonstrating that a generic drug delivers the same amount of active ingredient into a patient's bloodstream in the same timeframe as the brand-name counterpart, ensuring therapeutic equivalence. This scientific validation accelerates regulatory review processes, enabling faster market entry of cost-effective generic drugs that increase patient access to essential medications. Enhanced bioequivalence standards reduce variability in drug efficacy and safety, supporting public health objectives by expanding treatment options and lowering healthcare costs.
Future Trends in Bioequivalence and Generic Drug Evaluation
Future trends in bioequivalence and generic drug evaluation emphasize advanced modeling techniques such as physiologically based pharmacokinetic (PBPK) modeling and in vitro-in vivo correlation (IVIVC) to enhance predictive accuracy. Regulatory agencies are increasingly adopting real-world evidence and digital biomarkers to streamline approval processes while ensuring therapeutic equivalence. Innovations in nanotechnology and personalized medicine are driving the development of more precise bioequivalence assessments tailored to individual patient variability.
Bioequivalence and Generic Equivalence Infographic
 libterm.com
libterm.com