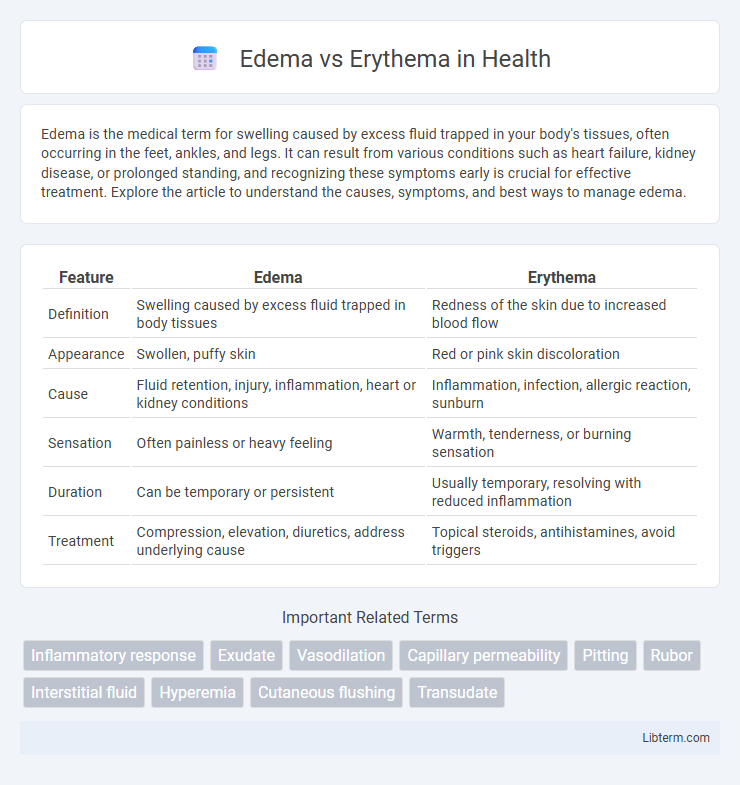
Edema is the medical term for swelling caused by excess fluid trapped in your body's tissues, often occurring in the feet, ankles, and legs. It can result from various conditions such as heart failure, kidney disease, or prolonged standing, and recognizing these symptoms early is crucial for effective treatment. Explore the article to understand the causes, symptoms, and best ways to manage edema.
Table of Comparison
| Feature | Edema | Erythema |
|---|---|---|
| Definition | Swelling caused by excess fluid trapped in body tissues | Redness of the skin due to increased blood flow |
| Appearance | Swollen, puffy skin | Red or pink skin discoloration |
| Cause | Fluid retention, injury, inflammation, heart or kidney conditions | Inflammation, infection, allergic reaction, sunburn |
| Sensation | Often painless or heavy feeling | Warmth, tenderness, or burning sensation |
| Duration | Can be temporary or persistent | Usually temporary, resolving with reduced inflammation |
| Treatment | Compression, elevation, diuretics, address underlying cause | Topical steroids, antihistamines, avoid triggers |
Understanding Edema: Definition and Causes
Edema refers to the abnormal accumulation of fluid in the interstitial spaces, leading to swelling, commonly caused by conditions such as heart failure, kidney disease, or localized injury. It results from increased hydrostatic pressure, decreased oncotic pressure, or lymphatic obstruction, disrupting normal fluid balance. Accurate identification of edema is crucial for diagnosing underlying systemic or localized disorders.
What is Erythema? Key Characteristics
Erythema is a medical condition characterized by redness of the skin caused by increased blood flow in superficial capillaries. Key characteristics include localized or diffuse redness, warmth, and sometimes swelling or tenderness, often resulting from inflammation, infection, or irritation. Unlike edema, which is swelling caused by fluid accumulation, erythema primarily involves vascular changes leading to visible skin redness.
Pathophysiology: How Edema and Erythema Occur
Edema occurs due to the accumulation of excess interstitial fluid caused by increased capillary hydrostatic pressure, decreased oncotic pressure, or lymphatic obstruction, leading to tissue swelling. Erythema results from the vasodilation of superficial blood vessels and increased blood flow in the skin, often triggered by inflammation, infection, or allergic reactions. Both conditions involve vascular changes, but edema is primarily fluid imbalance, whereas erythema reflects increased blood flow and vessel permeability.
Common Symptoms: Differentiating Edema from Erythema
Edema commonly presents as localized swelling caused by fluid accumulation in tissues, often accompanied by a feeling of tightness or heaviness in the affected area. Erythema is characterized by redness and warmth of the skin resulting from increased blood flow or inflammation, with symptoms including visible redness and sometimes slight swelling but primarily discoloration. Differentiating edema from erythema involves assessing the presence of swelling and fluid retention for edema versus skin redness and warmth for erythema.
Underlying Medical Conditions Associated with Edema and Erythema
Edema is commonly associated with underlying medical conditions such as congestive heart failure, chronic kidney disease, and liver cirrhosis, which lead to fluid retention and swelling. Erythema often indicates inflammatory or infectious processes linked to conditions like cellulitis, lupus erythematosus, or allergic reactions. Identifying the distinct causes of edema and erythema allows targeted diagnosis and treatment of underlying systemic diseases.
Diagnostic Approaches for Edema and Erythema
Diagnostic approaches for edema primarily involve clinical examination to identify swelling, palpation to assess pitting, and imaging techniques such as ultrasound or MRI to evaluate fluid accumulation. For erythema, diagnosis often relies on visual inspection of skin redness, dermoscopy to observe vascular patterns, and skin biopsy if inflammatory or infectious causes are suspected. Laboratory tests, including complete blood count and inflammatory markers, support differentiation between edema caused by systemic conditions and erythema resulting from dermatological or allergic reactions.
Risk Factors and Triggers
Edema risk factors include heart failure, kidney disease, liver cirrhosis, and prolonged immobility, while triggers often involve high salt intake, medication side effects, and injury. Erythema risk factors involve inflammatory conditions like dermatitis, infections, and autoimmune diseases, with triggers such as allergens, irritants, UV exposure, and physical trauma. Understanding these specific risk factors and triggers aids in differentiating diagnosis and guiding appropriate treatments.
Treatment Options: Edema vs Erythema
Treatment options for edema primarily include compression therapy, elevation of the affected area, and diuretics to reduce fluid accumulation. Erythema treatment focuses on addressing the underlying cause, such as antibiotics for infections or corticosteroids for inflammatory conditions, alongside soothing topical agents to reduce redness. Both conditions may require lifestyle changes and medical interventions tailored to the severity and root cause for effective management.
Complications and Prognosis
Edema can lead to complications such as impaired tissue perfusion, increased risk of infection, and chronic swelling that may result in permanent skin changes or ulceration. Erythema, often a sign of underlying inflammation or infection, can progress to complications like cellulitis, systemic infection, or tissue necrosis if untreated. Prognosis for edema depends on the cause and severity, with timely management reducing risks, while erythema prognosis varies widely based on the underlying condition and response to therapy.
Prevention and When to Seek Medical Care
Preventing edema involves maintaining proper hydration, reducing salt intake, engaging in regular physical activity, and avoiding prolonged periods of immobility to promote healthy circulation. To prevent erythema, protect skin from excessive sun exposure using sunscreen, wear protective clothing, and avoid known irritants or allergens that trigger inflammation. Seek medical care for edema if swelling is sudden, painful, accompanied by shortness of breath, or involves the chest, while erythema warrants urgent evaluation if redness spreads rapidly, is associated with fever, severe pain, or signs of infection.
Edema Infographic
 libterm.com
libterm.com