Natriuresis is the process by which the kidneys excrete excess sodium through the urine, playing a crucial role in regulating blood pressure and fluid balance. This mechanism helps your body maintain homeostasis by controlling sodium levels and preventing fluid retention. Explore the rest of the article to understand how natriuresis impacts your health and what factors influence this vital process.
Table of Comparison
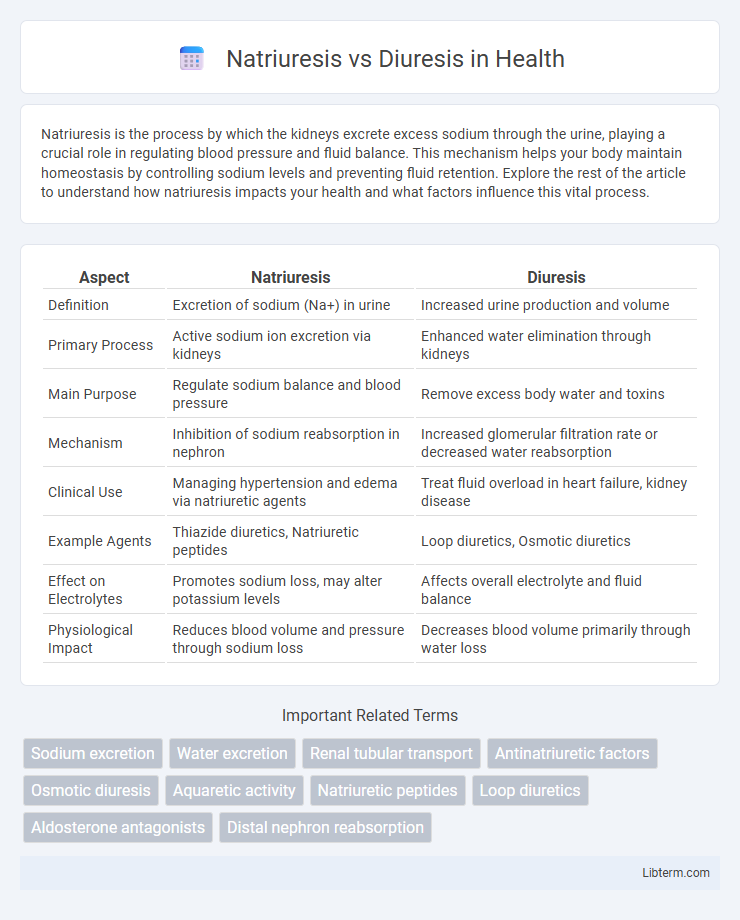
| Aspect | Natriuresis | Diuresis |
|---|---|---|
| Definition | Excretion of sodium (Na+) in urine | Increased urine production and volume |
| Primary Process | Active sodium ion excretion via kidneys | Enhanced water elimination through kidneys |
| Main Purpose | Regulate sodium balance and blood pressure | Remove excess body water and toxins |
| Mechanism | Inhibition of sodium reabsorption in nephron | Increased glomerular filtration rate or decreased water reabsorption |
| Clinical Use | Managing hypertension and edema via natriuretic agents | Treat fluid overload in heart failure, kidney disease |
| Example Agents | Thiazide diuretics, Natriuretic peptides | Loop diuretics, Osmotic diuretics |
| Effect on Electrolytes | Promotes sodium loss, may alter potassium levels | Affects overall electrolyte and fluid balance |
| Physiological Impact | Reduces blood volume and pressure through sodium loss | Decreases blood volume primarily through water loss |
Introduction to Natriuresis and Diuresis
Natriuresis refers to the excretion of sodium ions in the urine, a key mechanism regulating sodium balance and blood pressure in the body. Diuresis broadly describes the increased production of urine, which can result from various physiological or pharmacological factors influencing fluid elimination. Understanding the distinction between natriuresis and diuresis is crucial for clinical assessment of renal function and fluid-electrolyte homeostasis.
Definition of Natriuresis
Natriuresis refers to the process of excreting sodium ions (Na+) through the urine, which helps regulate sodium balance and blood pressure. Diuresis involves increased urine production without specifically targeting sodium excretion. The distinction lies in natriuresis promoting sodium removal, while diuresis primarily increases fluid output.
Definition of Diuresis
Diuresis refers to the increased production and excretion of urine by the kidneys, often triggered by factors such as fluid intake, medications, or underlying medical conditions. It plays a critical role in regulating electrolyte balance, blood pressure, and overall fluid volume in the body. Unlike natriuresis, which specifically involves excretion of sodium in the urine, diuresis encompasses the removal of water and solutes without necessarily altering sodium levels.
Mechanisms Underlying Natriuresis
Natriuresis involves the excretion of sodium in the urine, primarily regulated by the actions of natriuretic peptides such as atrial natriuretic peptide (ANP), which promote sodium excretion by increasing glomerular filtration rate and inhibiting sodium reabsorption in the renal tubules. This mechanism contrasts with diuresis, which primarily refers to increased urine volume resulting from enhanced water excretion, often without significant changes in sodium handling. Key renal transporters affected during natriuresis include the sodium-chloride symporter and the epithelial sodium channel, both of which are downregulated to facilitate sodium loss.
Mechanisms Underlying Diuresis
Diuresis primarily involves increased urine production through enhanced renal excretion of water, driven by factors such as osmotic gradients, hormonal regulation, and tubular reabsorption modulation. The mechanisms underlying diuresis include the inhibition of sodium and water reabsorption in different nephron segments, influenced by diuretics acting on the proximal tubule, loop of Henle, distal tubule, and collecting duct. Antidiuretic hormone (ADH) suppression also contributes to diuresis by reducing aquaporin channels in the collecting ducts, promoting free water clearance.
Key Differences Between Natriuresis and Diuresis
Natriuresis refers to the excretion of sodium in the urine, whereas diuresis involves an increased production of urine regardless of its sodium content. The key difference lies in natriuresis specifically promoting sodium loss to regulate blood pressure and fluid balance, while diuresis primarily increases urine volume to remove excess fluids. Understanding these processes is crucial for managing conditions like hypertension and edema, where sodium and fluid levels must be precisely controlled.
Clinical Significance of Natriuresis
Natriuresis involves the excretion of sodium in the urine, playing a critical role in regulating blood volume and pressure, with significant clinical implications for managing hypertension and heart failure. Monitoring natriuresis helps assess kidney function and the effectiveness of diuretic therapies, particularly loop and thiazide diuretics that promote sodium loss to reduce fluid overload. Unlike diuresis, which refers broadly to increased urine output, natriuresis specifically targets sodium balance and provides a more precise indicator of renal sodium handling and cardiovascular health.
Clinical Significance of Diuresis
Diuresis refers to the increased production of urine primarily through enhanced renal excretion of water, critical in managing fluid overload conditions such as heart failure and hypertension. Unlike natriuresis, which emphasizes sodium elimination, diuresis facilitates the removal of excess fluid, reducing edema and pulmonary congestion. Understanding diuresis is essential in clinical practice for optimizing diuretic therapy, monitoring electrolyte balance, and preventing complications like dehydration or renal impairment.
Common Conditions Involving Natriuresis and Diuresis
Common conditions involving natriuresis include congestive heart failure and hypertension, where excessive sodium excretion helps regulate fluid balance and blood pressure. Diuresis is prominently observed in diabetes insipidus and chronic kidney disease, characterized by increased urine output to eliminate excess water. Both processes play critical roles in electrolyte homeostasis and fluid regulation during conditions like edema and renal dysfunction.
Summary: Natriuresis vs Diuresis
Natriuresis refers to the excretion of sodium in the urine, playing a crucial role in regulating sodium balance and blood pressure by reducing extracellular fluid volume. Diuresis involves the increased production and excretion of urine, primarily affecting water balance and overall fluid volume without specifically targeting sodium. Understanding the distinction between natriuresis and diuresis is essential for managing conditions related to fluid overload, hypertension, and kidney function.
Natriuresis Infographic
 libterm.com
libterm.com