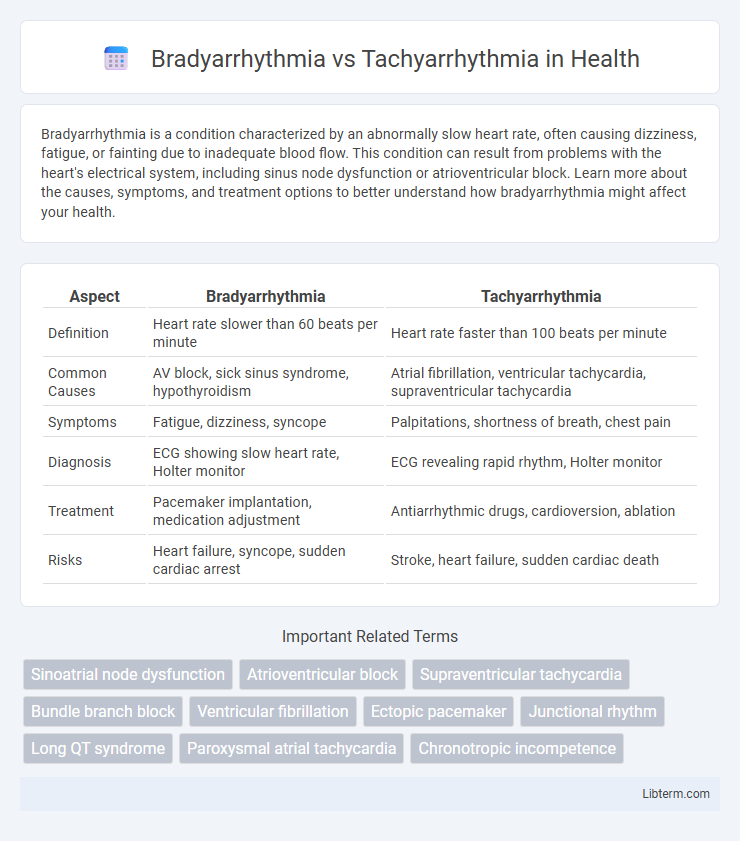
Bradyarrhythmia is a condition characterized by an abnormally slow heart rate, often causing dizziness, fatigue, or fainting due to inadequate blood flow. This condition can result from problems with the heart's electrical system, including sinus node dysfunction or atrioventricular block. Learn more about the causes, symptoms, and treatment options to better understand how bradyarrhythmia might affect your health.
Table of Comparison
| Aspect | Bradyarrhythmia | Tachyarrhythmia |
|---|---|---|
| Definition | Heart rate slower than 60 beats per minute | Heart rate faster than 100 beats per minute |
| Common Causes | AV block, sick sinus syndrome, hypothyroidism | Atrial fibrillation, ventricular tachycardia, supraventricular tachycardia |
| Symptoms | Fatigue, dizziness, syncope | Palpitations, shortness of breath, chest pain |
| Diagnosis | ECG showing slow heart rate, Holter monitor | ECG revealing rapid rhythm, Holter monitor |
| Treatment | Pacemaker implantation, medication adjustment | Antiarrhythmic drugs, cardioversion, ablation |
| Risks | Heart failure, syncope, sudden cardiac arrest | Stroke, heart failure, sudden cardiac death |
Introduction to Cardiac Arrhythmias
Bradyarrhythmia and tachyarrhythmia represent two primary categories of cardiac arrhythmias characterized by abnormal heart rhythms, with bradyarrhythmia involving a heart rate below 60 beats per minute and tachyarrhythmia exceeding 100 beats per minute. These conditions result from disruptions in the heart's electrical conduction system, affecting atrial, ventricular, or nodal tissues. Understanding the pathophysiology and clinical implications of bradyarrhythmia and tachyarrhythmia is essential for effective diagnosis and management of cardiac rhythm disorders.
Defining Bradyarrhythmia
Bradyarrhythmia is a cardiac rhythm disorder characterized by a slower-than-normal heart rate, typically fewer than 60 beats per minute, resulting from impaired electrical conduction in the sinoatrial node or atrioventricular node. This condition may lead to symptoms such as dizziness, fatigue, or syncope due to inadequate cardiac output. In contrast, tachyarrhythmia involves an abnormally fast heart rate that exceeds 100 beats per minute, often caused by abnormal excitability or automaticity in cardiac tissues.
Understanding Tachyarrhythmia
Tachyarrhythmia is characterized by abnormally fast heart rhythms typically exceeding 100 beats per minute, often resulting from electrical disturbances in the atria or ventricles. Common types include atrial fibrillation, atrial flutter, and ventricular tachycardia, each presenting unique risks for stroke, heart failure, and sudden cardiac arrest. Accurate diagnosis through ECG monitoring and timely intervention using medications, ablation therapy, or implantable devices is critical for managing tachyarrhythmia and preventing serious complications.
Key Differences Between Bradyarrhythmia and Tachyarrhythmia
Bradyarrhythmia is characterized by a heart rate below 60 beats per minute, often caused by sinus node dysfunction or atrioventricular block, leading to symptoms like fatigue and dizziness. Tachyarrhythmia involves a heart rate exceeding 100 beats per minute, commonly due to atrial fibrillation, ventricular tachycardia, or supraventricular tachycardia, resulting in palpitations and shortness of breath. The primary difference lies in the heart rate abnormalities, with bradyarrhythmias indicating abnormally slow rhythms and tachyarrhythmias reflecting abnormally fast rhythms, each requiring distinct diagnostic and therapeutic approaches.
Common Causes of Bradyarrhythmia
Bradyarrhythmia commonly results from sinus node dysfunction, atrioventricular block, or medication effects such as beta-blockers and calcium channel blockers. Structural heart diseases, including ischemic heart disease and cardiomyopathies, frequently contribute to impaired electrical conduction causing slow heart rates. Electrolyte imbalances and hypothyroidism are also notable metabolic contributors to bradyarrhythmia development.
Common Causes of Tachyarrhythmia
Tachyarrhythmia commonly arises from conditions such as atrial fibrillation, ventricular tachycardia, and supraventricular tachycardia, often triggered by electrolyte imbalances, ischemic heart disease, or hyperthyroidism. Other prevalent causes include congenital heart defects, stimulant use, and autonomic nervous system imbalances. Recognizing these etiologies is crucial for effective diagnosis and management of rapid heart rhythm disorders.
Clinical Manifestations and Symptoms
Bradyarrhythmia typically presents with symptoms such as fatigue, dizziness, syncope, and shortness of breath due to decreased heart rate and inadequate cardiac output. Tachyarrhythmia manifests through palpitations, chest pain, diaphoresis, and lightheadedness, often resulting from abnormally fast heart rhythms that impair cardiac efficiency. Both conditions can lead to hemodynamic instability, but the clinical presentation varies based on the heart rate deviation and underlying cardiac pathology.
Diagnostic Approaches
Electrocardiography (ECG) serves as the primary diagnostic tool for distinguishing Bradyarrhythmia, characterized by a heart rate below 60 beats per minute, from Tachyarrhythmia, where heart rates exceed 100 beats per minute. Holter monitoring and event recorders provide extended rhythm analysis essential for identifying intermittent arrhythmias that may not appear during standard ECG. Advanced techniques like electrophysiological studies (EPS) help localize arrhythmic foci and assess conduction pathways to guide targeted therapy.
Treatment Strategies for Each Condition
Treatment strategies for bradyarrhythmia typically involve addressing the underlying cause and may include pacemaker implantation to maintain adequate heart rate. Tachyarrhythmia management often requires antiarrhythmic medications, catheter ablation, or electrical cardioversion to restore normal rhythm and prevent complications. Both conditions demand tailored approaches based on patient-specific factors, arrhythmia type, and severity to optimize cardiac function and reduce morbidity.
Prognosis and Long-Term Management
Bradyarrhythmia prognosis depends on the underlying cause and severity, with pacemaker implantation often required for symptomatic cases to ensure stable heart rates and improve survival. Tachyarrhythmia prognosis varies by type, with atrial fibrillation linked to increased stroke risk, necessitating long-term anticoagulation and rhythm control strategies to reduce complications. Both conditions require ongoing monitoring, lifestyle modifications, and tailored pharmacologic or device therapies to optimize long-term outcomes and prevent progression or recurrent events.
Bradyarrhythmia Infographic
 libterm.com
libterm.com