Hyperoxia occurs when your body tissues are exposed to an excess supply of oxygen, often resulting from medical treatments or environmental exposure. While oxygen is vital for cellular function, too much can lead to oxidative stress, damaging cells and impairing organ function. Discover how understanding hyperoxia can help you recognize its risks and benefits by reading the remainder of this article.
Table of Comparison
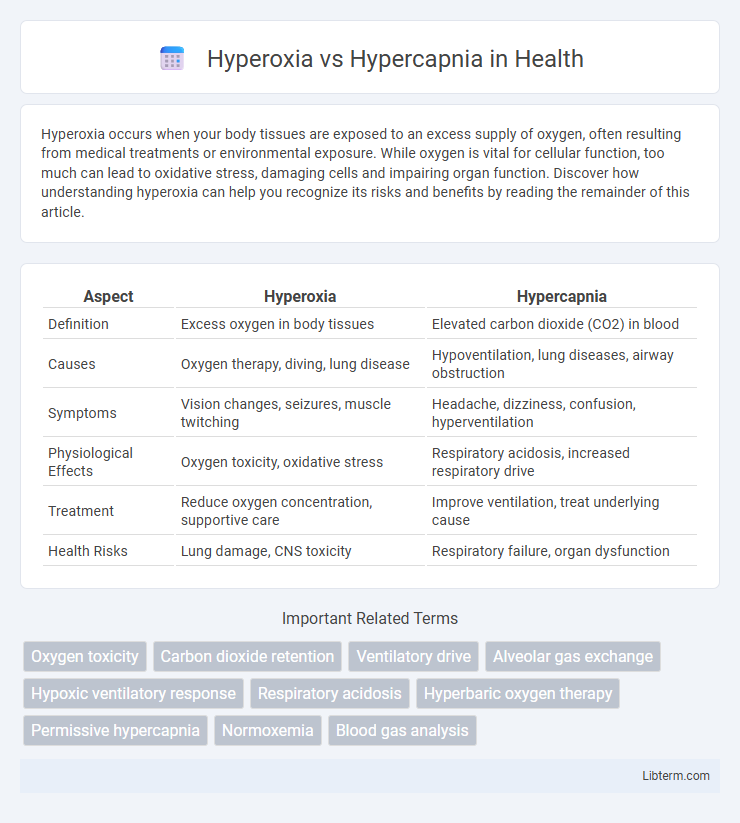
| Aspect | Hyperoxia | Hypercapnia |
|---|---|---|
| Definition | Excess oxygen in body tissues | Elevated carbon dioxide (CO2) in blood |
| Causes | Oxygen therapy, diving, lung disease | Hypoventilation, lung diseases, airway obstruction |
| Symptoms | Vision changes, seizures, muscle twitching | Headache, dizziness, confusion, hyperventilation |
| Physiological Effects | Oxygen toxicity, oxidative stress | Respiratory acidosis, increased respiratory drive |
| Treatment | Reduce oxygen concentration, supportive care | Improve ventilation, treat underlying cause |
| Health Risks | Lung damage, CNS toxicity | Respiratory failure, organ dysfunction |
Introduction to Hyperoxia and Hypercapnia
Hyperoxia refers to an excessive oxygen level in body tissues, typically caused by inhaling oxygen-rich air or medical oxygen therapy, leading to oxidative stress and potential cellular damage. Hypercapnia involves elevated carbon dioxide (CO2) concentrations in the bloodstream, commonly resulting from hypoventilation or respiratory disorders, disrupting acid-base balance and causing respiratory acidosis. Both conditions significantly affect respiratory and metabolic functions, warranting careful monitoring during clinical treatment.
Understanding Oxygen and Carbon Dioxide Levels
Hyperoxia occurs when oxygen levels in the blood exceed normal physiological ranges, often measured as arterial partial pressure of oxygen (PaO2) above 100 mmHg, leading to potential oxidative stress and cellular damage. Hypercapnia refers to elevated carbon dioxide levels in the bloodstream, indicated by increased arterial partial pressure of carbon dioxide (PaCO2) above 45 mmHg, contributing to respiratory acidosis and altered blood pH. Monitoring and regulating PaO2 and PaCO2 are critical in clinical settings to maintain homeostasis and prevent complications associated with imbalanced oxygen and carbon dioxide levels.
Causes of Hyperoxia
Hyperoxia occurs when there is an excessive amount of oxygen in the blood, commonly caused by medical interventions such as supplemental oxygen therapy or hyperbaric oxygen treatment. It can also result from environmental exposure to high oxygen levels or oxygen-rich gas mixtures, particularly in intensive care units or aviation settings. Prolonged hyperoxia leads to oxidative stress and cellular damage, highlighting the importance of carefully controlling oxygen administration to prevent complications.
Causes of Hypercapnia
Hypercapnia is primarily caused by hypoventilation, where inadequate ventilation leads to insufficient removal of carbon dioxide from the lungs. Respiratory conditions such as chronic obstructive pulmonary disease (COPD), asthma, and obstructive sleep apnea significantly contribute to the accumulation of CO2. Other causes include neuromuscular disorders that impair respiratory muscle function and diseases affecting the central nervous system's respiratory control centers.
Physiological Effects of Hyperoxia
Hyperoxia results in elevated oxygen levels in the blood, leading to vasoconstriction, especially in cerebral and coronary arteries, which can reduce blood flow despite increased oxygen content. Excess oxygen generates reactive oxygen species (ROS), causing oxidative stress that damages cellular lipids, proteins, and DNA. Prolonged hyperoxia may impair lung function through inflammation and alveolar injury, highlighting the importance of balanced oxygen therapy.
Physiological Impacts of Hypercapnia
Hypercapnia, characterized by elevated carbon dioxide levels in the blood, disrupts acid-base balance by causing respiratory acidosis and stimulates chemoreceptors to increase ventilation. It leads to vasodilation, increased intracranial pressure, and can depress central nervous system function if severe. Unlike hyperoxia, which primarily causes oxidative stress and tissue damage, hypercapnia directly affects respiratory drive and cardiovascular regulation.
Clinical Manifestations and Symptoms
Hyperoxia and hypercapnia present distinct clinical manifestations; hyperoxia often causes symptoms such as visual disturbances, muscle twitching, and seizures due to oxygen toxicity, while hypercapnia leads to headache, confusion, flushed skin, and dyspnea resulting from elevated carbon dioxide levels in the blood. In hyperoxia cases, patients may exhibit pulmonary symptoms including coughing and difficulty breathing, whereas hypercapnia is frequently associated with respiratory acidosis, causing increased heart rate and elevated blood pressure. Early recognition of these symptoms is critical in managing underlying causes and preventing severe complications such as respiratory failure or cerebral edema.
Diagnosis and Monitoring Techniques
Hyperoxia diagnosis primarily relies on arterial blood gas (ABG) analysis to measure elevated partial pressure of oxygen (PaO2) levels, often above 100 mmHg, while pulse oximetry can monitor oxygen saturation continuously. Hypercapnia is identified through ABG showing increased partial pressure of carbon dioxide (PaCO2) above 45 mmHg, with capnography serving as a valuable real-time monitoring tool for end-tidal CO2 levels in respiratory management. Both conditions require frequent evaluation using non-invasive methods like transcutaneous CO2 monitoring or continuous SpO2 to prevent complications associated with improper oxygen or carbon dioxide levels.
Treatment and Management Strategies
Treatment of hyperoxia involves reducing supplemental oxygen to prevent oxygen toxicity and oxidative stress, often by titrating oxygen to maintain target saturation levels between 92-96%. Management of hypercapnia focuses on improving ventilation through non-invasive positive pressure ventilation (NIPPV) or mechanical ventilation to enhance carbon dioxide elimination. Both conditions require continuous monitoring of arterial blood gases and respiratory function to adjust therapy and prevent complications.
Preventive Measures and Best Practices
Preventive measures for hyperoxia emphasize monitoring oxygen levels using pulse oximetry and adjusting supplemental oxygen to maintain target SpO2 between 92-96%, avoiding excess oxygen administration. Best practices for hypercapnia prevention include ensuring adequate ventilation through mechanical or spontaneous means, regular arterial blood gas analysis, and managing underlying respiratory conditions to promote effective CO2 elimination. Both conditions require individualized patient assessment, continuous monitoring, and adherence to clinical guidelines to minimize risks and optimize respiratory function.
Hyperoxia Infographic
 libterm.com
libterm.com