Infarction occurs when blood supply to a part of the body, often the heart or brain, is blocked, leading to tissue damage or death due to oxygen deprivation. Recognizing early signs and understanding risk factors such as atherosclerosis, smoking, and high blood pressure can be crucial for prevention and timely treatment. Explore this article to learn more about the causes, symptoms, and management of infarction to protect your health.
Table of Comparison
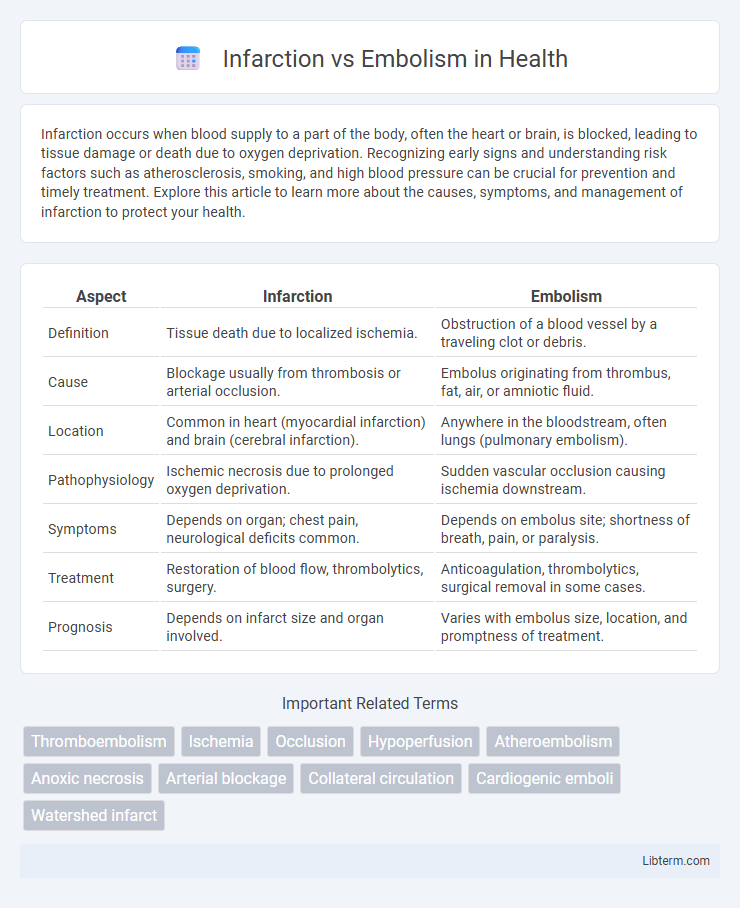
| Aspect | Infarction | Embolism |
|---|---|---|
| Definition | Tissue death due to localized ischemia. | Obstruction of a blood vessel by a traveling clot or debris. |
| Cause | Blockage usually from thrombosis or arterial occlusion. | Embolus originating from thrombus, fat, air, or amniotic fluid. |
| Location | Common in heart (myocardial infarction) and brain (cerebral infarction). | Anywhere in the bloodstream, often lungs (pulmonary embolism). |
| Pathophysiology | Ischemic necrosis due to prolonged oxygen deprivation. | Sudden vascular occlusion causing ischemia downstream. |
| Symptoms | Depends on organ; chest pain, neurological deficits common. | Depends on embolus site; shortness of breath, pain, or paralysis. |
| Treatment | Restoration of blood flow, thrombolytics, surgery. | Anticoagulation, thrombolytics, surgical removal in some cases. |
| Prognosis | Depends on infarct size and organ involved. | Varies with embolus size, location, and promptness of treatment. |
Understanding Infarction: Definition and Mechanism
Infarction refers to tissue death caused by an inadequate blood supply due to the obstruction of blood vessels, commonly resulting from thrombosis or embolism. The mechanism involves ischemia-induced cellular injury, leading to necrosis within the affected area, typically in organs like the heart, brain, or lungs. Understanding the pathophysiology of infarction is crucial for discerning its clinical manifestations and guiding appropriate treatment strategies.
What is Embolism? Key Concepts Explained
Embolism is the sudden blockage of a blood vessel by an embolus, which is often a blood clot, fat globule, air bubble, or other foreign substance traveling through the bloodstream. This obstruction disrupts normal blood flow, potentially causing tissue damage or infarction downstream due to oxygen deprivation. Unlike infarction, which is the localized death of tissue caused by prolonged ischemia, embolism is the causative event leading to such ischemic damage.
Causes of Infarction: Common Triggers
Infarction commonly results from arterial occlusion caused by thrombosis, which is the most frequent trigger, restricting blood flow and leading to tissue ischemia. Embolism, another significant cause, involves the sudden blockage of vessels by emboli such as blood clots, fat globules, or air bubbles transported through the bloodstream. Other causes of infarction include vasospasm, external compression of vessels, and systemic hypoperfusion due to shock or cardiac failure.
Etiology of Embolism: Origins and Risk Factors
Embolism primarily originates from thrombi formed in the heart or large arteries, with atrial fibrillation and myocardial infarction being significant cardiac sources. Other origins include fat emboli from long bone fractures, air embolism from invasive procedures, and septic emboli from infected cardiac valves. Risk factors encompass hypercoagulable states, prolonged immobilization, atrial fibrillation, valvular heart disease, and atherosclerosis, all of which increase the likelihood of embolus formation and arterial occlusion.
Pathophysiology: How Infarction Differs from Embolism
Infarction results from localized tissue death due to prolonged ischemia caused by arterial occlusion, whereas embolism involves the sudden blockage of a blood vessel by an embolus that can be a blood clot, fat, air, or other debris. Pathophysiologically, infarction develops when the downstream tissue experiences oxygen deprivation, leading to cellular necrosis, while embolism initiates an acute interruption of blood flow that may cause infarction if collateral circulation fails. The key difference lies in infarction being the consequence of sustained ischemia and tissue necrosis, whereas embolism is the event causing acute vascular obstruction.
Clinical Manifestations: Signs and Symptoms Compared
Infarction typically presents with localized tissue necrosis leading to sudden severe pain, pallor, and loss of function in the affected area, reflecting compromised blood supply. Embolism often causes abrupt symptoms depending on the embolus location, such as stroke-like neurological deficits, chest pain in pulmonary embolism, or limb ischemia with cold, cyanotic extremities. Both conditions may show signs of systemic response like tachycardia and hypotension but differ mainly in the clinical pattern and onset of ischemic symptoms.
Diagnostic Approaches for Infarction and Embolism
Diagnostic approaches for infarction involve imaging techniques such as MRI and CT scans to identify tissue necrosis and ischemic zones, supplemented by blood tests assessing markers like troponins in myocardial infarction. Embolism diagnosis often requires Doppler ultrasound, angiography, and echocardiography to detect emboli location and source, alongside lab tests for clotting disorders or atrial fibrillation. Accurate differentiation relies on integrating clinical history, imaging findings, and coagulation profiles to tailor appropriate treatment strategies.
Treatment Strategies: Managing Infarction vs Embolism
Treatment strategies for infarction primarily focus on restoring blood flow through thrombolytic therapy or surgical intervention to remove the occlusion and limit tissue damage. Embolism management emphasizes prompt anticoagulation to prevent further clot propagation, with embolus removal or embolectomy considered in severe cases. Both conditions require tailored approaches based on the affected organ and the severity of ischemia to optimize patient outcomes.
Prognosis and Complications: Outcomes and Risks
Infarction prognosis depends on the size and location of the affected tissue, with larger infarcts leading to significant organ dysfunction and increased risk of heart failure or stroke. Embolism prognosis varies by the embolus origin and the vascular territory involved, often resulting in sudden ischemia with potential for rapid tissue death and secondary complications like infection or chronic pain. Both conditions carry risks of permanent damage, recurrent events, and impact on patient morbidity and mortality, necessitating prompt diagnosis and tailored management.
Prevention Tips: Reducing Infarction and Embolism Incidence
Effective prevention of infarction and embolism centers on managing cardiovascular risk factors such as hypertension, diabetes, and hyperlipidemia through lifestyle modifications and medication adherence. Regular physical activity, a balanced diet low in saturated fats, and smoking cessation significantly reduce the incidence of arterial blockages and thromboembolic events. Monitoring and controlling atrial fibrillation and using anticoagulant therapy when prescribed are vital in preventing embolic strokes and infarctions.
Infarction Infographic
 libterm.com
libterm.com