Bacterial vaginosis is a common vaginal infection caused by an imbalance of bacteria, leading to symptoms like unusual discharge and odor. Proper diagnosis and treatment are essential to prevent complications and restore healthy vaginal flora. Discover how you can effectively identify, manage, and prevent bacterial vaginosis by reading the rest of this article.
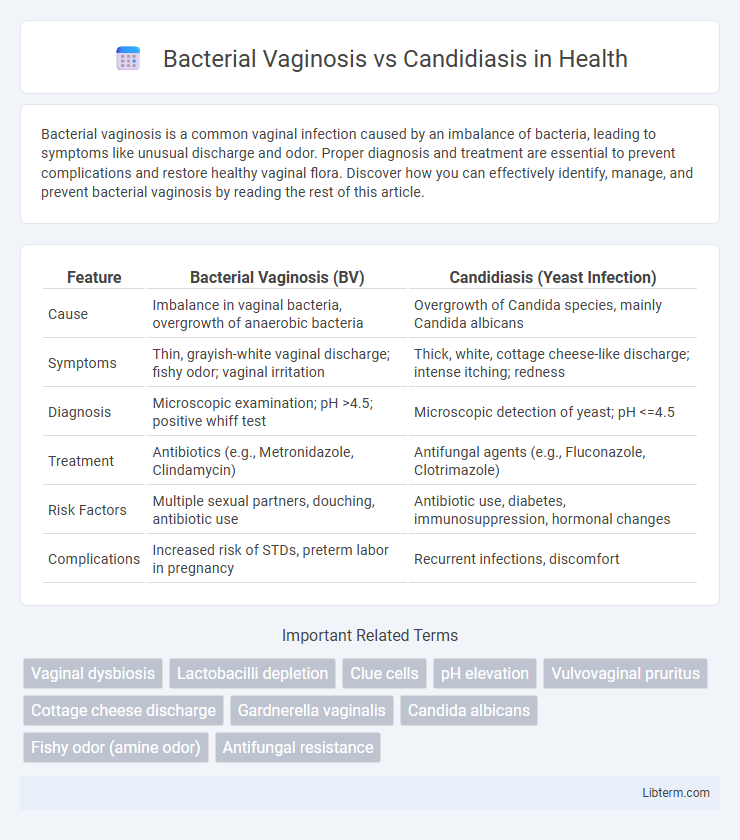
Table of Comparison
| Feature | Bacterial Vaginosis (BV) | Candidiasis (Yeast Infection) |
|---|---|---|
| Cause | Imbalance in vaginal bacteria, overgrowth of anaerobic bacteria | Overgrowth of Candida species, mainly Candida albicans |
| Symptoms | Thin, grayish-white vaginal discharge; fishy odor; vaginal irritation | Thick, white, cottage cheese-like discharge; intense itching; redness |
| Diagnosis | Microscopic examination; pH >4.5; positive whiff test | Microscopic detection of yeast; pH <=4.5 |
| Treatment | Antibiotics (e.g., Metronidazole, Clindamycin) | Antifungal agents (e.g., Fluconazole, Clotrimazole) |
| Risk Factors | Multiple sexual partners, douching, antibiotic use | Antibiotic use, diabetes, immunosuppression, hormonal changes |
| Complications | Increased risk of STDs, preterm labor in pregnancy | Recurrent infections, discomfort |
Introduction to Bacterial Vaginosis and Candidiasis
Bacterial Vaginosis (BV) is a common vaginal infection caused by an imbalance in the vaginal microbiota, characterized by a decrease in Lactobacillus species and an overgrowth of anaerobic bacteria such as Gardnerella vaginalis. Candidiasis, also known as a yeast infection, is primarily caused by the overgrowth of Candida species, especially Candida albicans, leading to itching, discharge, and inflammation. Both conditions affect vaginal health but differ significantly in their microbial etiology and treatment approaches.
Causes and Risk Factors
Bacterial vaginosis (BV) is primarily caused by an imbalance in the vaginal microbiota, particularly the overgrowth of Gardnerella vaginalis and a reduction in Lactobacillus species, often triggered by factors such as antibiotic use, douching, and multiple sexual partners. Candidiasis, commonly caused by Candida albicans, results from fungal overgrowth due to immune suppression, uncontrolled diabetes, antibiotic therapy, or hormonal changes like pregnancy. Both conditions share risk factors including the disruption of normal vaginal flora but differ fundamentally in their microbial etiologies and underlying causes.
Signs and Symptoms Comparison
Bacterial Vaginosis typically presents with a thin, grayish-white vaginal discharge accompanied by a fishy odor, especially after intercourse, and mild itching or irritation. Candidiasis, or vaginal yeast infection, is characterized by thick, white, cottage cheese-like discharge, intense itching, redness, and swelling of the vulva. Unlike Bacterial Vaginosis, Candidiasis often causes burning sensations during urination and sexual intercourse.
How Each Condition is Diagnosed
Bacterial vaginosis is diagnosed primarily through clinical examination and specific tests such as vaginal pH measurement above 4.5, the presence of clue cells in microscopic analysis, and a characteristic fishy odor detected with a whiff test. Candidiasis diagnosis involves microscopic identification of Candida species or yeast cells in vaginal discharge and may include fungal culture to confirm the infection. Both conditions utilize laboratory tests like microscopy and culture but differ in symptoms and specific diagnostic criteria related to their unique microbial causes.
Differences in Vaginal Discharge
Bacterial Vaginosis (BV) typically causes a thin, grayish-white vaginal discharge with a strong fishy odor, especially after intercourse. In contrast, Candidiasis, a yeast infection caused by Candida species, produces a thick, white, cottage cheese-like discharge that is usually odorless. These distinctive discharge characteristics are key diagnostic indicators distinguishing BV from candidiasis in clinical settings.
Treatment Options for Bacterial Vaginosis
Bacterial Vaginosis (BV) treatment primarily involves antibiotics such as metronidazole or clindamycin, which target the overgrowth of Gardnerella vaginalis and restore vaginal flora balance. Oral or topical administration methods are effective, with metronidazole gel reducing recurrence rates and clindamycin cream offering symptom relief. Probiotic therapy and lifestyle modifications may support long-term treatment outcomes by maintaining healthy lactobacilli populations in the vaginal microbiome.
Treatment Options for Candidiasis
Treatment options for candidiasis primarily include antifungal medications such as fluconazole, clotrimazole, and miconazole, available in oral or topical forms. Timely administration of these antifungal agents effectively eliminates Candida overgrowth, alleviating symptoms like itching, discharge, and irritation. Maintaining proper vaginal hygiene and avoiding irritants can help prevent recurrent candidiasis episodes.
Prevention Strategies for Both Infections
Preventing bacterial vaginosis involves maintaining a balanced vaginal microbiome by avoiding excessive antibiotic use and practicing good hygiene, such as wiping front to back and refraining from douching. Candidiasis prevention centers on controlling factors that promote yeast overgrowth, including managing blood sugar levels in diabetics, wearing breathable cotton underwear, and limiting the use of scented feminine products. Both infections benefit from safe sexual practices and timely treatment of any vaginal symptoms to reduce recurrence risk.
When to Seek Medical Attention
Seek medical attention for bacterial vaginosis when experiencing abnormal vaginal discharge with a fishy odor, itching, or burning during urination, as untreated BV can increase the risk of pelvic inflammatory disease and pregnancy complications. For candidiasis, consult a healthcare provider if intense itching, thick white vaginal discharge resembling cottage cheese, or redness and swelling persist despite over-the-counter antifungal treatments or if symptoms recur frequently. Early diagnosis and treatment are essential to prevent complications such as recurrent infections and to maintain vaginal health.
Frequently Asked Questions (FAQs)
Bacterial Vaginosis (BV) and Candidiasis are common vaginal infections with distinct causes; BV results from an imbalance of vaginal bacteria, while Candidiasis is caused by an overgrowth of the yeast Candida. Frequently asked questions often address symptoms such as abnormal discharge, odor in BV, and itching or thick white discharge in Candidiasis, as well as treatment options like antibiotics for BV and antifungal medications for Candidiasis. Understanding differences in diagnosis methods, risk factors, and recurrence rates helps in managing these infections effectively.
Bacterial Vaginosis Infographic
 libterm.com
libterm.com