Infections occur when harmful microorganisms invade your body, triggering immune responses that aim to eliminate the threat. Understanding the types, symptoms, and treatments of infections is crucial for effective prevention and recovery. Explore the rest of this article to learn more about how to protect yourself from infections and maintain your health.
Table of Comparison
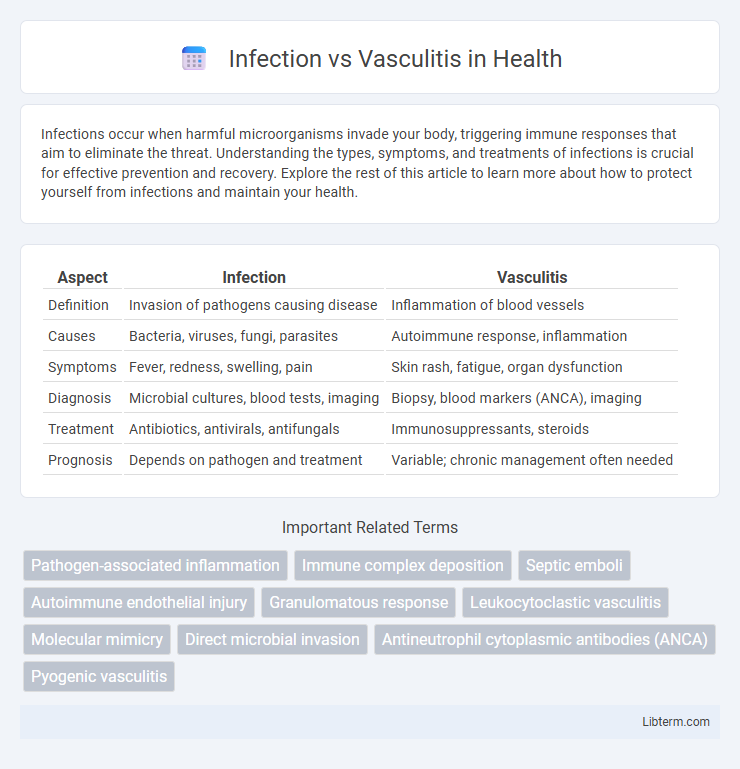
| Aspect | Infection | Vasculitis |
|---|---|---|
| Definition | Invasion of pathogens causing disease | Inflammation of blood vessels |
| Causes | Bacteria, viruses, fungi, parasites | Autoimmune response, inflammation |
| Symptoms | Fever, redness, swelling, pain | Skin rash, fatigue, organ dysfunction |
| Diagnosis | Microbial cultures, blood tests, imaging | Biopsy, blood markers (ANCA), imaging |
| Treatment | Antibiotics, antivirals, antifungals | Immunosuppressants, steroids |
| Prognosis | Depends on pathogen and treatment | Variable; chronic management often needed |
Understanding Infection and Vasculitis: Key Definitions
Infection involves the invasion and multiplication of pathogens such as bacteria, viruses, or fungi within body tissues, triggering inflammatory responses to eliminate the infectious agents. Vasculitis refers to the inflammation of blood vessel walls, which can result from autoimmune processes or secondary to infections, leading to blood flow disruption and tissue damage. Differentiating between infection-induced inflammation and primary vasculitis is critical for accurate diagnosis and targeted treatment, relying on clinical presentation, laboratory markers, and imaging studies.
Pathophysiology: How Infections Differ from Vasculitis
Infections trigger an immune response by pathogens such as bacteria, viruses, or fungi that directly invade tissues, causing inflammation and often producing pus or necrosis. Vasculitis involves inflammation of blood vessel walls primarily due to an autoimmune reaction, leading to vessel wall damage, ischemia, and tissue injury without direct microbial invasion. The pathophysiology of infection centers on pathogen-mediated tissue injury and immune clearance, whereas vasculitis is characterized by immune complex deposition, complement activation, and granulomatous inflammation targeting endothelial cells.
Common Causes: Infectious Agents vs. Immune Triggers
Infections are commonly caused by bacterial pathogens like Staphylococcus aureus and Streptococcus species, viral agents such as herpes simplex virus, and fungal organisms including Candida. Vasculitis, on the other hand, is often triggered by immune responses involving autoimmune diseases like systemic lupus erythematosus and granulomatosis with polyangiitis, as well as hypersensitivity to medications or chronic infections. Understanding these distinct etiologies aids in accurate diagnosis and targeted treatment strategies.
Signs and Symptoms: Distinguishing Clinical Features
Infections typically present with localized redness, warmth, swelling, and fever, often accompanied by purulent discharge or systemic signs such as increased white blood cell count. Vasculitis manifests with palpable purpura, ulcers, and glomerulonephritis symptoms due to inflammation of blood vessels, frequently accompanied by systemic features like weight loss and fatigue. Laboratory findings such as elevated inflammatory markers (ESR, CRP) and specific autoantibodies (ANCA) aid in distinguishing vasculitis from infectious causes.
Diagnostic Approaches: Laboratory and Imaging Differences
Infection diagnosis relies heavily on laboratory tests such as blood cultures, elevated white blood cell counts, and inflammatory markers like C-reactive protein (CRP) and procalcitonin, whereas vasculitis is typically identified through specific autoantibodies including antineutrophil cytoplasmic antibodies (ANCA) and erythrocyte sedimentation rate (ESR) elevation. Imaging modalities for infection often reveal abscesses or localized fluid collections on ultrasound, CT, or MRI, while vasculitis imaging detects vessel wall thickening, stenosis, or aneurysms, using angiography or PET scans to highlight inflammatory changes in blood vessels. Distinguishing features include the presence of pathogens in cultures for infections versus the immune-mediated vascular inflammation seen in vasculitis, guiding targeted treatment decisions.
Treatment Strategies: Antimicrobials vs. Immunosuppressives
Treatment strategies for infection primarily involve targeted antimicrobials such as antibiotics, antivirals, or antifungals to eradicate the causative pathogen and restore immune balance. In contrast, vasculitis management centers on immunosuppressive agents like corticosteroids, cyclophosphamide, or biologics to reduce inflammation and prevent vessel damage caused by aberrant immune responses. Accurate differential diagnosis is critical, as immunosuppression in infectious cases may exacerbate disease, while inappropriate antimicrobial use in vasculitis delays effective control of autoimmune inflammation.
Overlapping Manifestations: When Infection Mimics Vasculitis
Infection and vasculitis share overlapping clinical manifestations such as fever, fatigue, and elevated inflammatory markers, complicating differential diagnosis. Certain infections like bacterial endocarditis, tuberculosis, and viral hepatitis can mimic vasculitis by causing vessel inflammation and tissue damage. Accurate diagnosis relies on integrating microbiological cultures, serologic tests, imaging, and histopathology to distinguish infectious etiologies from autoimmune-driven vasculitis.
Complications: Risks Associated with Each Condition
Infections can lead to complications such as sepsis, abscess formation, and systemic inflammatory response syndrome (SIRS), posing significant risks of organ failure and prolonged hospital stays. Vasculitis complications include vessel stenosis, aneurysm formation, and ischemic damage due to impaired blood flow, which may result in tissue necrosis and organ dysfunction. Both conditions increase the risk of morbidity and require prompt diagnosis and targeted treatment to minimize these severe outcomes.
Prognosis: Outcomes in Infection and Vasculitis
Infections generally have a variable prognosis depending on the pathogen virulence, site of infection, and timeliness of antimicrobial therapy, with many cases resolving completely when treated promptly. Vasculitis prognosis depends on the type, extent of vascular involvement, and response to immunosuppressive therapy, with some forms leading to chronic organ damage or relapses. Early diagnosis and targeted management significantly improve outcomes in both infection-related and vasculitic conditions, reducing morbidity and mortality rates.
Prevention and Monitoring: Reducing Misdiagnosis
Effective prevention of infection and vasculitis involves timely vaccination, proper hygiene, and avoiding known triggers such as autoimmune predispositions or environmental factors. Monitoring combines regular clinical evaluation with targeted laboratory tests including inflammatory markers, blood cultures, and imaging studies to distinguish infectious causes from inflammatory vasculitis. Accurate differentiation minimizes misdiagnosis, ensuring appropriate treatment by leveraging biomarkers like C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and specific autoantibodies such as antineutrophil cytoplasmic antibodies (ANCA).
Infection Infographic
 libterm.com
libterm.com