Glossitis is an inflammation of the tongue characterized by swelling, redness, and a smooth appearance due to the loss of papillae. It can result from infections, nutritional deficiencies, allergies, or irritants, impacting your ability to taste and speak comfortably. Discover the causes, symptoms, and effective treatments for glossitis by reading the full article.
Table of Comparison
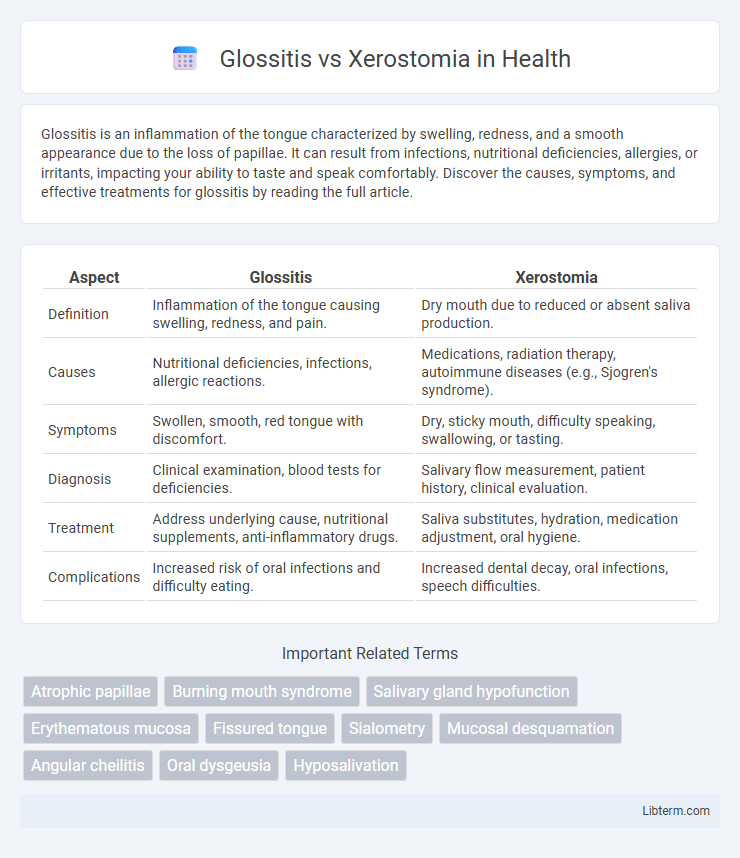
| Aspect | Glossitis | Xerostomia |
|---|---|---|
| Definition | Inflammation of the tongue causing swelling, redness, and pain. | Dry mouth due to reduced or absent saliva production. |
| Causes | Nutritional deficiencies, infections, allergic reactions. | Medications, radiation therapy, autoimmune diseases (e.g., Sjogren's syndrome). |
| Symptoms | Swollen, smooth, red tongue with discomfort. | Dry, sticky mouth, difficulty speaking, swallowing, or tasting. |
| Diagnosis | Clinical examination, blood tests for deficiencies. | Salivary flow measurement, patient history, clinical evaluation. |
| Treatment | Address underlying cause, nutritional supplements, anti-inflammatory drugs. | Saliva substitutes, hydration, medication adjustment, oral hygiene. |
| Complications | Increased risk of oral infections and difficulty eating. | Increased dental decay, oral infections, speech difficulties. |
Introduction to Glossitis and Xerostomia
Glossitis is an inflammatory condition characterized by the swelling, redness, and smooth appearance of the tongue, often caused by nutritional deficiencies, infections, or allergic reactions. Xerostomia, commonly known as dry mouth, results from reduced or absent saliva flow, frequently linked to medications, autoimmune diseases like Sjogren's syndrome, or radiation therapy. Both conditions significantly impact oral health, affecting speech, taste, and the ability to chew and swallow.
Defining Glossitis: Causes and Symptoms
Glossitis is an inflammatory condition characterized by swelling, redness, and a smooth appearance of the tongue, often caused by nutritional deficiencies such as vitamin B12 or iron, infections, allergic reactions, or irritants like tobacco. Patients commonly experience pain, burning sensations, and changes in taste sensation, with the tongue appearing shiny and swollen due to papillae atrophy. Differentiating glossitis from xerostomia, which primarily involves dry mouth due to reduced saliva production, is essential for targeted diagnosis and treatment.
Understanding Xerostomia: Causes and Symptoms
Xerostomia, commonly known as dry mouth, results from reduced or absent saliva production and is often caused by medications, autoimmune diseases such as Sjogren's syndrome, or radiation therapy targeting the head and neck. Symptoms include a sticky or dry feeling in the mouth, difficulties in speaking, chewing, swallowing, and an increased risk of dental decay and oral infections. Understanding these causes and symptoms is crucial for effective management and distinguishing xerostomia from conditions like glossitis, which involves inflammation of the tongue.
Key Differences Between Glossitis and Xerostomia
Glossitis is characterized by inflammation of the tongue, causing redness, swelling, and changes in the tongue's texture, often linked to nutritional deficiencies or infections. Xerostomia, or dry mouth, results from reduced saliva production, leading to dryness, difficulty swallowing, and increased risk of dental decay. Unlike glossitis, which primarily affects the tongue's surface, xerostomia impacts oral moisture and overall oral health by impairing saliva function.
Common Risk Factors for Glossitis and Xerostomia
Common risk factors for glossitis and xerostomia include nutritional deficiencies such as vitamin B12, iron, and folate, which contribute to inflammation of the tongue and reduced saliva production. Chronic illnesses like diabetes, autoimmune disorders, and infections also predispose individuals to both conditions. Medications including antihypertensives, antidepressants, and chemotherapy agents frequently cause dry mouth and tongue inflammation as side effects.
Diagnostic Approaches for Glossitis vs Xerostomia
Diagnostic approaches for glossitis primarily involve clinical examination of the tongue for characteristics such as swelling, redness, and loss of papillae, combined with patient history to identify underlying causes like nutritional deficiencies or infections. In contrast, xerostomia diagnosis relies on subjective patient reports of dry mouth symptoms, salivary flow rate measurements, and tests such as sialometry or salivary gland imaging to assess salivary gland function. Laboratory tests including blood work or biopsy may support diagnosis for both conditions by identifying systemic diseases or infections contributing to glossitis or xerostomia.
Treatment Options for Glossitis
Treatment options for glossitis primarily involve addressing the underlying cause, such as nutritional deficiencies, infections, or irritants. Supplementation with iron, vitamin B12, or folic acid is often effective when deficiencies are identified, while antifungal or antibiotic medications target infectious causes. Symptomatic relief may include topical corticosteroids or analgesic gels to reduce inflammation and discomfort.
Management Strategies for Xerostomia
Management strategies for xerostomia primarily involve stimulating saliva production and maintaining oral moisture. Patients are advised to use saliva substitutes, chew sugar-free gum or lozenges containing xylitol, and stay well-hydrated by drinking water frequently. In more severe cases, prescription medications such as pilocarpine or cevimeline can be administered to enhance salivary gland function and alleviate dry mouth symptoms.
Prevention Tips for Glossitis and Xerostomia
Maintaining proper oral hygiene and staying hydrated are essential prevention tips for glossitis and xerostomia. Avoiding irritants such as tobacco, alcohol, and spicy foods can reduce the risk of glossitis and help manage dry mouth symptoms. Regular dental check-ups and a balanced diet rich in vitamins, particularly B-complex and iron, support oral mucosa health and saliva production.
When to Seek Professional Dental Care
Seek professional dental care immediately if symptoms of glossitis, such as swollen, smooth, or painful tongue, are persistent or worsen beyond two weeks, as it may indicate underlying nutritional deficiencies or infections. For xerostomia, consult a dentist if dry mouth causes difficulty swallowing, persistent bad breath, or increased tooth decay risk, since untreated saliva reduction can lead to severe oral health complications. Early diagnosis and treatment by a dental professional help prevent progression of these conditions and manage potential systemic health issues.
Glossitis Infographic
 libterm.com
libterm.com