Osteomyelitis is a severe bone infection caused by bacteria or fungi that leads to inflammation and destruction of bone tissue. Early diagnosis and treatment, including antibiotics or surgery, are crucial to prevent chronic complications and preserve bone health. Explore the rest of the article to understand the symptoms, diagnosis, and effective treatment options for osteomyelitis.
Table of Comparison
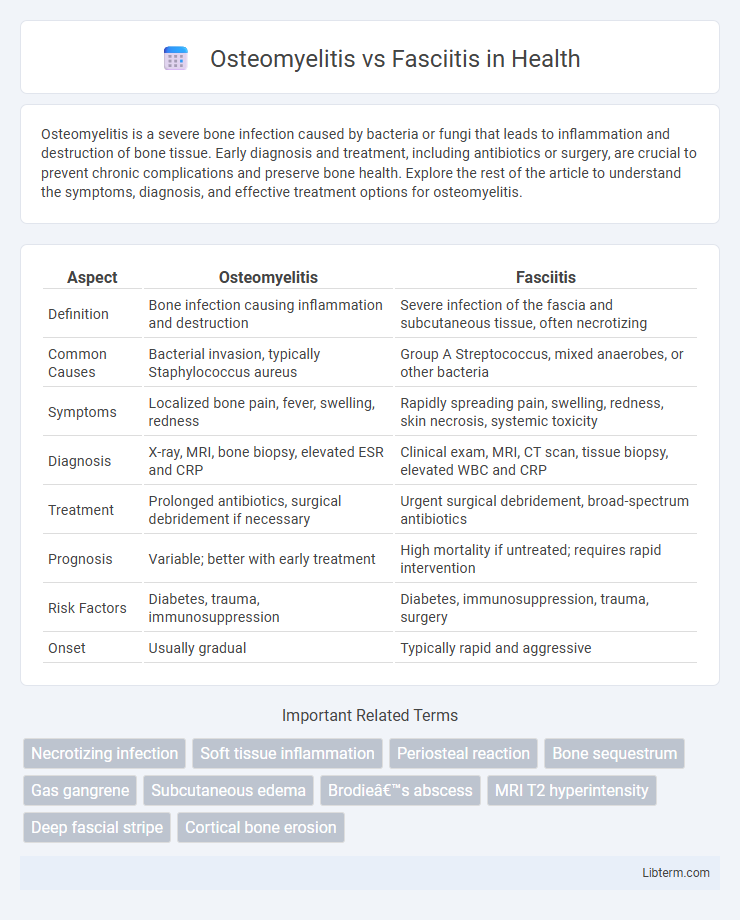
| Aspect | Osteomyelitis | Fasciitis |
|---|---|---|
| Definition | Bone infection causing inflammation and destruction | Severe infection of the fascia and subcutaneous tissue, often necrotizing |
| Common Causes | Bacterial invasion, typically Staphylococcus aureus | Group A Streptococcus, mixed anaerobes, or other bacteria |
| Symptoms | Localized bone pain, fever, swelling, redness | Rapidly spreading pain, swelling, redness, skin necrosis, systemic toxicity |
| Diagnosis | X-ray, MRI, bone biopsy, elevated ESR and CRP | Clinical exam, MRI, CT scan, tissue biopsy, elevated WBC and CRP |
| Treatment | Prolonged antibiotics, surgical debridement if necessary | Urgent surgical debridement, broad-spectrum antibiotics |
| Prognosis | Variable; better with early treatment | High mortality if untreated; requires rapid intervention |
| Risk Factors | Diabetes, trauma, immunosuppression | Diabetes, immunosuppression, trauma, surgery |
| Onset | Usually gradual | Typically rapid and aggressive |
Overview: Osteomyelitis vs Fasciitis
Osteomyelitis is a severe bone infection caused by bacteria or fungi, often resulting in inflammation and bone destruction, while fasciitis refers to inflammation of the fascia, the connective tissue surrounding muscles, frequently leading to severe soft tissue infections like necrotizing fasciitis. Osteomyelitis typically develops from open wounds, surgery, or bloodstream infections, characterized by localized bone pain, fever, and swelling, whereas fasciitis manifests with rapid tissue destruction, intense pain, redness, and systemic symptoms such as fever and shock. Accurate diagnosis through imaging and microbiological tests is crucial, as treatment for osteomyelitis often involves prolonged antibiotics and possible surgical debridement, while fasciitis requires urgent surgical intervention and broad-spectrum antibiotics to prevent life-threatening complications.
Definition and Etiology
Osteomyelitis is a severe bone infection typically caused by bacteria such as Staphylococcus aureus, resulting in inflammation and bone destruction. Fasciitis, particularly necrotizing fasciitis, is a rapidly progressing bacterial infection affecting the fascia and subcutaneous tissues, commonly caused by Group A Streptococcus or polymicrobial flora. Both conditions involve infectious agents but differ in tissue targets, with osteomyelitis affecting bone and fasciitis targeting connective soft tissue.
Pathophysiology Differences
Osteomyelitis primarily involves infection and inflammation of the bone marrow and cortical bone, leading to bone destruction caused by hematogenous spread, direct inoculation, or contiguous spread from adjacent tissues. In contrast, fasciitis, particularly necrotizing fasciitis, affects the superficial and deep fascia with rapid bacterial invasion and toxin production, resulting in widespread tissue necrosis and systemic toxicity. The distinct pathophysiology lies in osteomyelitis targeting osseous structures with compromised vascular supply, while fasciitis aggressively targets fascial planes and soft tissues, often progressing more rapidly.
Risk Factors and Predisposing Conditions
Osteomyelitis primarily occurs in individuals with diabetes, immunosuppression, recent trauma, or invasive orthopedic procedures, increasing susceptibility to bone infections. Fasciitis, particularly necrotizing fasciitis, is commonly associated with immunocompromised states, chronic illnesses like diabetes and peripheral vascular disease, and injuries that breach skin integrity. Both conditions share risk factors such as compromised immunity and poor wound healing, but fasciitis often progresses rapidly due to bacterial toxin production in soft tissue, while osteomyelitis involves localized bone infection with slower onset.
Clinical Presentation
Osteomyelitis typically presents with localized bone pain, swelling, warmth, and fever, often accompanied by reduced limb function, whereas fasciitis, such as necrotizing fasciitis, manifests with severe, rapidly progressing soft tissue pain, erythema, swelling, and systemic toxicity. Laboratory findings in osteomyelitis may show elevated inflammatory markers like ESR and CRP, while fasciitis often demonstrates signs of systemic infection including leukocytosis and hypotension. Imaging studies for osteomyelitis reveal bone destruction or periosteal reaction, contrasting with fasciitis which shows soft tissue gas and edema on MRI or CT scans.
Diagnostic Approaches
Osteomyelitis diagnosis relies on imaging techniques such as MRI and CT scans, alongside blood tests for inflammatory markers and bone biopsy for definitive microbial identification. Fasciitis diagnosis emphasizes clinical evaluation, supported by MRI to detect fascial inflammation and may require surgical exploration for confirmation. Early differentiation through targeted imaging and laboratory analysis is crucial to guide appropriate treatment strategies for these infections.
Imaging and Laboratory Findings
Osteomyelitis typically presents on imaging with bone destruction, periosteal reaction, and possible sequestra on X-rays, while MRI is more sensitive in detecting early marrow edema and abscess formation. Laboratory findings in osteomyelitis often reveal elevated white blood cell count (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), with blood cultures positive in many cases. In contrast, fasciitis, especially necrotizing fasciitis, shows diffuse soft tissue swelling, gas formation along fascial planes on CT or MRI, and laboratory markers demonstrate elevated CRP, leukocytosis, and severe metabolic acidosis, often requiring prompt surgical evaluation.
Treatment Options and Management
Osteomyelitis treatment typically involves prolonged antibiotic therapy guided by culture results and, in severe cases, surgical debridement to remove necrotic bone tissue. Fasciitis, especially necrotizing fasciitis, requires urgent surgical intervention for aggressive debridement combined with broad-spectrum intravenous antibiotics to control rapid soft tissue infection. Management of both conditions includes supportive care, monitoring for complications, and tailored antibiotic regimens based on pathogen sensitivity and infection severity.
Complications and Prognosis
Osteomyelitis often leads to chronic bone infection, which can cause bone necrosis, chronic pain, and potential spread to surrounding joints, resulting in long-term functional impairment. Fasciitis, particularly necrotizing fasciitis, has a rapid progression with high risk of systemic toxicity, sepsis, and multi-organ failure, demanding urgent medical intervention. Prognosis for osteomyelitis improves with early antibiotic therapy and surgical debridement, while fasciitis carries a guarded prognosis due to its aggressive nature and potential for widespread tissue destruction.
Prevention and Patient Education
Effective prevention of osteomyelitis and fasciitis centers on early wound care, maintaining good hygiene, and managing underlying conditions like diabetes to reduce infection risk. Patient education should emphasize recognizing early symptoms such as localized pain, swelling, redness, or fever and seeking prompt medical evaluation to prevent disease progression. Proper vaccination, avoiding high-risk injuries, and adherence to prescribed antibiotics are crucial strategies to minimize complications associated with these infections.
Osteomyelitis Infographic
 libterm.com
libterm.com