Hyponatremia occurs when sodium levels in your blood drop below normal, causing symptoms like headache, nausea, and confusion due to cellular swelling. It often results from excessive water intake, certain medications, or underlying medical conditions affecting fluid balance. Explore the rest of the article to understand causes, symptoms, and effective treatments for managing hyponatremia.
Table of Comparison
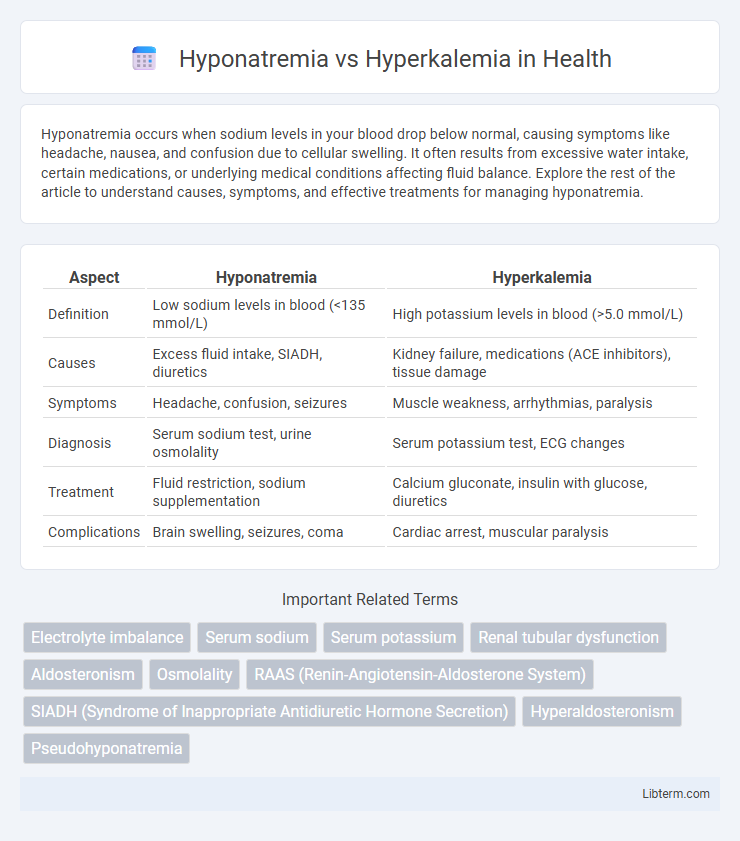
| Aspect | Hyponatremia | Hyperkalemia |
|---|---|---|
| Definition | Low sodium levels in blood (<135 mmol/L) | High potassium levels in blood (>5.0 mmol/L) |
| Causes | Excess fluid intake, SIADH, diuretics | Kidney failure, medications (ACE inhibitors), tissue damage |
| Symptoms | Headache, confusion, seizures | Muscle weakness, arrhythmias, paralysis |
| Diagnosis | Serum sodium test, urine osmolality | Serum potassium test, ECG changes |
| Treatment | Fluid restriction, sodium supplementation | Calcium gluconate, insulin with glucose, diuretics |
| Complications | Brain swelling, seizures, coma | Cardiac arrest, muscular paralysis |
Understanding Hyponatremia: Definition and Causes
Hyponatremia is a condition characterized by low sodium concentration in the blood, typically below 135 mmol/L, leading to symptoms like confusion, headache, and seizures. Common causes include excessive water intake, heart failure, kidney disease, and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Understanding the pathophysiology involves recognizing sodium's vital role in maintaining fluid balance and nerve function, where an imbalance disrupts cellular processes and can result in life-threatening complications.
Hyperkalemia Explained: Key Causes and Risk Factors
Hyperkalemia, characterized by elevated potassium levels in the blood above 5.0 mmol/L, results primarily from impaired kidney function, excessive potassium intake, or cellular shifts caused by acidosis or tissue damage. Risk factors include chronic kidney disease, use of potassium-sparing diuretics or ACE inhibitors, adrenal insufficiency, and conditions like diabetes mellitus that affect potassium regulation. Monitoring serum potassium and managing underlying causes are critical to prevent severe cardiac complications associated with hyperkalemia.
Pathophysiological Differences Between Hyponatremia and Hyperkalemia
Hyponatremia results from a relative excess of water compared to sodium in the extracellular fluid, causing cellular swelling due to hypotonicity and leading to neurologic symptoms. Hyperkalemia arises from impaired renal potassium excretion, cellular release, or increased potassium intake, disturbing the resting membrane potential and causing cardiac arrhythmias. The distinct pathophysiology in hyponatremia involves sodium dilution and water imbalance, whereas hyperkalemia primarily affects potassium homeostasis and cellular excitability.
Common Symptoms: Hyponatremia vs Hyperkalemia
Hyponatremia commonly presents with nausea, headache, confusion, and in severe cases, seizures or coma due to low sodium levels affecting neurological function. Hyperkalemia symptoms include muscle weakness, fatigue, palpitations, and potentially life-threatening cardiac arrhythmias caused by elevated potassium levels. Both conditions require prompt diagnosis and management to prevent serious complications.
Diagnostic Criteria and Laboratory Assessment
Hyponatremia is diagnosed when serum sodium levels fall below 135 mEq/L, often confirmed through plasma osmolality and urine sodium tests to differentiate causes such as hypovolemia or syndrome of inappropriate antidiuretic hormone secretion (SIADH). Hyperkalemia is identified by serum potassium levels exceeding 5.0 mEq/L, with laboratory assessment including electrocardiogram changes and evaluation of renal function, acid-base balance, and medications influencing potassium homeostasis. Both conditions require precise laboratory analysis of electrolyte panels, serum osmolality, and clinical correlation for accurate diagnosis and management.
Treatment Strategies for Hyponatremia
Treatment strategies for hyponatremia primarily involve addressing the underlying cause while carefully correcting serum sodium levels to avoid osmotic demyelination syndrome. Management includes fluid restriction in cases of dilutional hyponatremia, administration of hypertonic saline for severe symptomatic cases, and use of vasopressin receptor antagonists (vaptans) in syndrome of inappropriate antidiuretic hormone secretion (SIADH). Monitoring electrolyte levels and patient response closely ensures safe normalization of sodium without rapid shifts.
Managing Hyperkalemia: Current Approaches
Managing hyperkalemia involves rapid assessment and treatment to prevent life-threatening cardiac arrhythmias. Current approaches prioritize stabilizing the cardiac membrane with intravenous calcium gluconate, shifting potassium intracellularly using insulin with glucose or beta-2 agonists, and removing excess potassium through diuretics, sodium polystyrene sulfonate, or dialysis. Continuous monitoring of serum potassium levels and ECG changes is critical for effective hyperkalemia management and prevention of complications.
Potential Complications: What to Watch For
Hyponatremia can lead to cerebral edema, seizures, and even coma due to rapid shifts in brain cell osmolarity, while hyperkalemia poses a high risk of cardiac arrhythmias, muscle weakness, and potential cardiac arrest because of its effects on myocardial excitability. Monitoring electrocardiogram changes such as peaked T waves in hyperkalemia and neurological symptoms like confusion or lethargy in hyponatremia is crucial for early detection and management. Timely intervention based on laboratory electrolyte levels and clinical presentation reduces the risk of life-threatening complications in both disorders.
Prevention and Risk Reduction Tips
Hyponatremia prevention focuses on maintaining proper sodium balance through adequate salt intake and avoiding excessive water consumption, especially in athletes or those with kidney issues. Hyperkalemia risk reduction includes monitoring potassium-rich foods, managing medications like ACE inhibitors, and controlling underlying conditions such as chronic kidney disease or diabetes. Regular blood tests and careful electrolyte management are essential for early detection and prevention of complications in both disorders.
Clinical Case Comparisons: Hyponatremia vs Hyperkalemia
Hyponatremia typically presents with symptoms such as nausea, headache, confusion, and seizures due to low serum sodium levels below 135 mEq/L, whereas hyperkalemia manifests with muscle weakness, fatigue, and potentially life-threatening cardiac arrhythmias from elevated potassium levels above 5.0 mEq/L. Clinical case comparisons highlight that hyponatremia often results from fluid imbalance disorders like syndrome of inappropriate antidiuretic hormone secretion (SIADH), while hyperkalemia commonly arises in cases of kidney failure, adrenal insufficiency, or use of potassium-sparing diuretics. Effective management requires accurate diagnosis through serum electrolyte panels and tailored interventions, such as sodium correction in hyponatremia and emergency treatments like calcium gluconate or insulin with glucose for hyperkalemia-induced cardiac toxicity.
Hyponatremia Infographic
 libterm.com
libterm.com