Rheumatoid arthritis is a chronic autoimmune disorder that primarily affects the joints, causing inflammation, pain, and swelling that can lead to joint damage and loss of function. Effective management includes a combination of medication, physical therapy, and lifestyle adjustments tailored to reduce symptoms and improve quality of life. Discover practical strategies and in-depth insights to help you better understand and manage rheumatoid arthritis in the rest of this article.
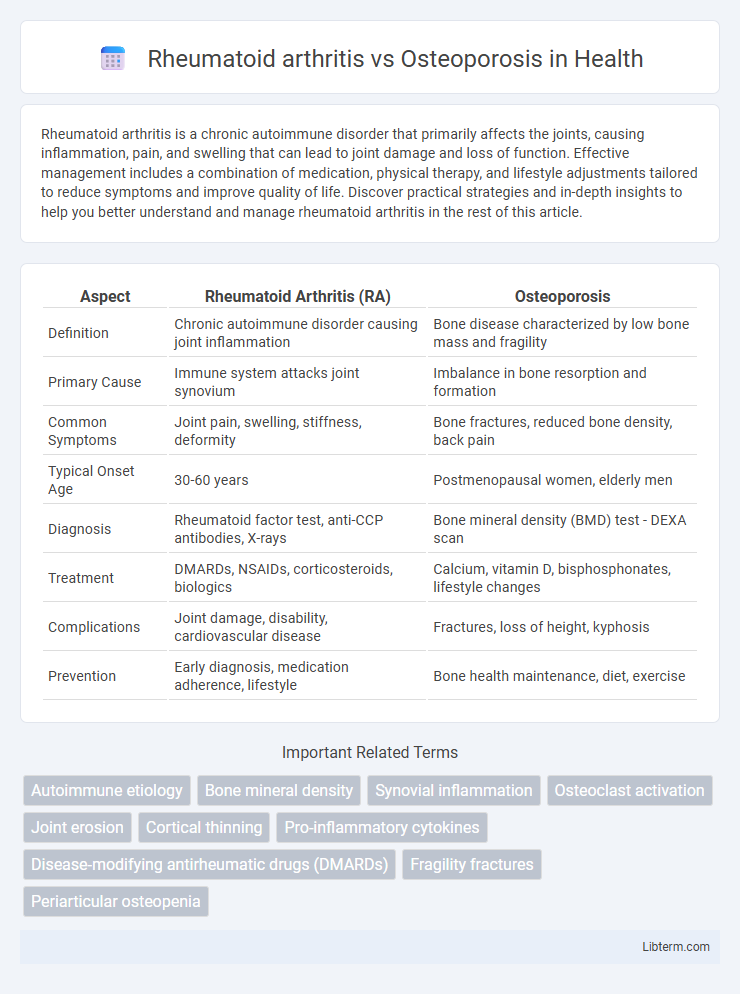
Table of Comparison
| Aspect | Rheumatoid Arthritis (RA) | Osteoporosis |
|---|---|---|
| Definition | Chronic autoimmune disorder causing joint inflammation | Bone disease characterized by low bone mass and fragility |
| Primary Cause | Immune system attacks joint synovium | Imbalance in bone resorption and formation |
| Common Symptoms | Joint pain, swelling, stiffness, deformity | Bone fractures, reduced bone density, back pain |
| Typical Onset Age | 30-60 years | Postmenopausal women, elderly men |
| Diagnosis | Rheumatoid factor test, anti-CCP antibodies, X-rays | Bone mineral density (BMD) test - DEXA scan |
| Treatment | DMARDs, NSAIDs, corticosteroids, biologics | Calcium, vitamin D, bisphosphonates, lifestyle changes |
| Complications | Joint damage, disability, cardiovascular disease | Fractures, loss of height, kyphosis |
| Prevention | Early diagnosis, medication adherence, lifestyle | Bone health maintenance, diet, exercise |
Introduction to Rheumatoid Arthritis and Osteoporosis
Rheumatoid arthritis is a chronic autoimmune disorder characterized by inflammation of the joints, leading to pain, swelling, and potential joint deformity. Osteoporosis is a metabolic bone disease marked by decreased bone density and increased fracture risk, primarily due to imbalance in bone resorption and formation. Both conditions commonly affect older adults but differ fundamentally in pathophysiology and treatment approaches.
Causes and Risk Factors
Rheumatoid arthritis is an autoimmune disorder primarily caused by genetic predisposition and environmental triggers such as smoking and infections, leading to chronic joint inflammation. Osteoporosis results from an imbalance between bone resorption and formation, with key risk factors including aging, hormonal changes (especially decreased estrogen in postmenopausal women), calcium deficiency, and sedentary lifestyle. Both diseases increase with age, but rheumatoid arthritis is linked to immune system dysregulation, whereas osteoporosis is driven by bone metabolism deterioration.
Symptoms Comparison
Rheumatoid arthritis primarily causes joint pain, swelling, stiffness, and reduced mobility, often affecting hands and feet symmetrically, with morning stiffness lasting over an hour. Osteoporosis is characterized by decreased bone density, leading to fragile bones, height loss, and an increased risk of fractures, often without pain until a fracture occurs. Unlike rheumatoid arthritis, osteoporosis typically lacks inflammation and joint symptoms but presents with fractures commonly in the hip, spine, and wrist.
Disease Progression
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation and progressive joint destruction, often leading to deformities and loss of function if untreated. Osteoporosis involves the gradual loss of bone density and microarchitecture degradation, increasing fracture risk over time without prominent inflammatory symptoms. Both diseases progress differently, with RA primarily causing joint damage due to synovial inflammation, while osteoporosis results in systemic skeletal fragility due to decreased bone mass.
Diagnosis Methods
Rheumatoid arthritis diagnosis primarily involves clinical evaluation, blood tests for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, and imaging techniques like X-rays, MRI, or ultrasound to detect joint inflammation and damage. Osteoporosis diagnosis relies on bone mineral density (BMD) measurement using dual-energy X-ray absorptiometry (DEXA or DXA) scans, which assess bone strength and fracture risk. Both conditions may include laboratory tests, but imaging remains central to confirming rheumatoid arthritis and osteoporosis accurately.
Treatment Options
Rheumatoid arthritis treatment primarily involves disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, biologics like TNF inhibitors, and corticosteroids to reduce inflammation and prevent joint damage. Osteoporosis management focuses on bisphosphonates, calcium and vitamin D supplementation, and lifestyle modifications to enhance bone density and reduce fracture risk. Both conditions require tailored therapies based on severity, with regular monitoring to optimize patient outcomes.
Impact on Daily Life
Rheumatoid arthritis significantly impairs daily life by causing joint pain, stiffness, and swelling, which limit mobility and dexterity, affecting activities such as dressing, cooking, and typing. Osteoporosis increases fracture risk due to bone fragility, leading to reduced independence and mobility after falls or fractures, particularly in the hip, spine, and wrist. Both conditions demand careful management to maintain quality of life, but rheumatoid arthritis often involves continuous pain and inflammation, while osteoporosis impacts become pronounced primarily after bone injury.
Prevention Strategies
Effective prevention strategies for rheumatoid arthritis focus on maintaining a healthy lifestyle, including regular exercise, a balanced diet rich in anti-inflammatory foods, and avoiding smoking to reduce autoimmune triggers. Osteoporosis prevention emphasizes adequate calcium and vitamin D intake, weight-bearing physical activity, and lifestyle modifications such as limiting alcohol consumption and avoiding sedentary behavior to maintain bone density. Early screening and risk assessment are crucial for both conditions to implement personalized prevention plans and minimize long-term complications.
Long-Term Complications
Rheumatoid arthritis can cause long-term complications such as joint deformity, chronic pain, and increased risk of cardiovascular disease due to systemic inflammation. Osteoporosis primarily leads to an elevated risk of fractures, especially in the hip, spine, and wrist, which can result in decreased mobility and disability. Both conditions require management strategies to minimize bone damage and preserve quality of life over time.
Key Differences and Similarities
Rheumatoid arthritis primarily affects the joints causing inflammation, swelling, and pain, while osteoporosis is characterized by reduced bone density and increased fracture risk. Both conditions disproportionately impact older adults and can lead to decreased mobility and quality of life. Immune system dysfunction drives rheumatoid arthritis, whereas osteoporosis results mainly from bone resorption exceeding bone formation.
Rheumatoid arthritis Infographic
 libterm.com
libterm.com