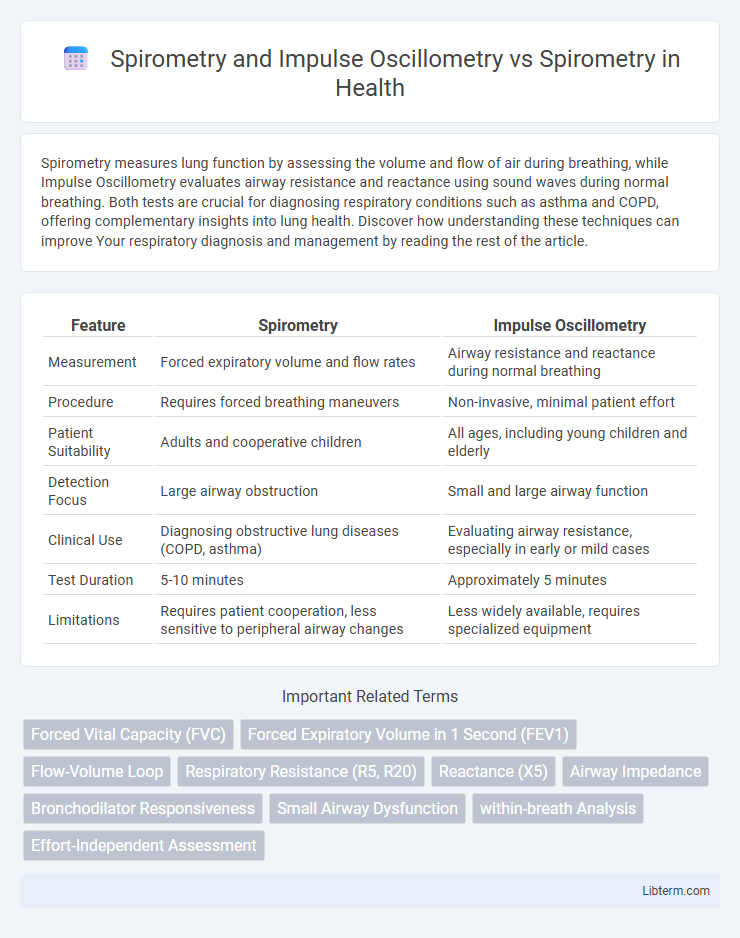
Spirometry measures lung function by assessing the volume and flow of air during breathing, while Impulse Oscillometry evaluates airway resistance and reactance using sound waves during normal breathing. Both tests are crucial for diagnosing respiratory conditions such as asthma and COPD, offering complementary insights into lung health. Discover how understanding these techniques can improve Your respiratory diagnosis and management by reading the rest of the article.
Table of Comparison
| Feature | Spirometry | Impulse Oscillometry |
|---|---|---|
| Measurement | Forced expiratory volume and flow rates | Airway resistance and reactance during normal breathing |
| Procedure | Requires forced breathing maneuvers | Non-invasive, minimal patient effort |
| Patient Suitability | Adults and cooperative children | All ages, including young children and elderly |
| Detection Focus | Large airway obstruction | Small and large airway function |
| Clinical Use | Diagnosing obstructive lung diseases (COPD, asthma) | Evaluating airway resistance, especially in early or mild cases |
| Test Duration | 5-10 minutes | Approximately 5 minutes |
| Limitations | Requires patient cooperation, less sensitive to peripheral airway changes | Less widely available, requires specialized equipment |
Introduction to Pulmonary Function Testing
Pulmonary function testing (PFT) encompasses various techniques like spirometry and impulse oscillometry (IOS) to assess respiratory health. Spirometry measures airflow and lung volumes during forceful breathing maneuvers, providing critical data on obstructive and restrictive lung diseases. Impulse oscillometry offers a non-invasive, effort-independent method to evaluate airway resistance and reactance, enhancing early detection of small airway dysfunction alongside traditional spirometry.
Understanding Spirometry: Principles and Applications
Spirometry measures lung function by assessing airflow and volume during forced breathing maneuvers, providing critical data on obstructive and restrictive respiratory conditions. Impulse Oscillometry complements spirometry by evaluating airway resistance and reactance using sound waves during normal breathing, enhancing detection of small airway abnormalities. Understanding spirometry principles allows clinicians to accurately interpret parameters like FEV1, FVC, and FEV1/FVC ratio for diagnosis and management of pulmonary diseases.
What is Impulse Oscillometry?
Impulse Oscillometry (IOS) is a non-invasive respiratory test that measures lung function by assessing airway resistance and reactance using sound waves during normal breathing. Unlike traditional Spirometry, which requires forceful exhalation and measures airflow and lung volumes, IOS evaluates small airway function with minimal patient effort, making it suitable for children and those unable to perform spirometry maneuvers. IOS provides detailed insights into airway mechanics, aiding in early detection of obstructive and restrictive lung diseases.
Key Differences: Impulse Oscillometry vs Spirometry
Impulse Oscillometry (IOS) measures airway resistance and reactance during normal tidal breathing, providing detailed assessment of small airway function, unlike Spirometry which requires forced maneuvers to evaluate lung volumes and airflow rates. IOS is highly sensitive for early detection of peripheral airway obstruction and is easier to perform in young children or patients with severe respiratory conditions compared to Spirometry. Spirometry remains the gold standard for diagnosing obstructive and restrictive lung diseases, whereas IOS offers complementary data on respiratory mechanics, particularly in heterogeneous airway diseases such as asthma and COPD.
Clinical Indications for Spirometry
Spirometry is primarily indicated for diagnosing and monitoring obstructive and restrictive lung diseases such as asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis. It measures forced expiratory volume and forced vital capacity to assess airflow limitation and lung function impairment. Impulse Oscillometry complements spirometry by providing detailed information on airway resistance and reactance, especially useful in patients unable to perform forced maneuvers.
Advantages of Impulse Oscillometry in Respiratory Assessment
Impulse Oscillometry (IOS) offers enhanced sensitivity in detecting small airway dysfunction and peripheral airway resistance compared to Spirometry, making it especially useful in early-stage respiratory diseases like asthma and COPD. IOS requires minimal patient effort and cooperation, enabling accurate assessments in young children, elderly patients, or individuals unable to perform forced respiratory maneuvers. Additionally, IOS provides detailed information on respiratory system mechanics during normal tidal breathing, facilitating more comprehensive and patient-friendly respiratory evaluations.
Limitations of Spirometry and Impulse Oscillometry
Spirometry, the gold standard for assessing lung function, is limited by its dependence on patient effort and coordination, which can lead to variability in results and difficulty in use among children or elderly patients. Impulse Oscillometry (IOS) offers a less effort-dependent alternative by measuring respiratory system impedance during normal tidal breathing, yet it faces limitations in widespread clinical adoption due to less standardized reference values and lower availability. Both methods complement each other, with spirometry providing detailed airflow measurements while IOS better detects small airway dysfunction, especially in patients unable to perform forced maneuvers.
Comparative Accuracy: Detecting Small Airway Disease
Impulse Oscillometry (IOS) offers superior sensitivity in detecting small airway disease compared to Spirometry by measuring airway resistance and reactance at multiple frequencies, providing detailed insights into peripheral airway function. Spirometry primarily assesses larger airway obstruction through forced expiratory volumes, which may overlook subtle changes in the small airways. Studies demonstrate that IOS parameters, such as reactance at 5 Hz (X5) and frequency dependence of resistance (R5-R20), exhibit enhanced accuracy in early diagnosis and monitoring of small airway involvement in conditions like asthma and COPD.
Patient Suitability and Comfort Considerations
Impulse Oscillometry (IOS) requires minimal patient effort and is especially suitable for young children, elderly patients, and individuals with severe respiratory muscle weakness, enhancing comfort and compliance. In contrast, Spirometry demands active patient cooperation and maximal effort, which may be challenging for those populations, potentially affecting test accuracy and patient comfort. IOS provides detailed airway resistance data during normal tidal breathing, making it a more patient-friendly option for vulnerable groups compared to the forced expiratory maneuvers required in Spirometry.
Future Perspectives in Pulmonary Diagnostics
Future perspectives in pulmonary diagnostics emphasize the integration of Spirometry and Impulse Oscillometry to enhance early detection and monitoring of respiratory diseases. Impulse Oscillometry, offering sensitive assessment of small airway function with minimal patient effort, complements Spirometry's measurement of airflow and lung volumes, enabling more comprehensive pulmonary evaluation. Advances in digital health technologies and AI-driven analytics are poised to refine interpretation accuracy and facilitate personalized treatment strategies based on combined Spirometry and Oscillometry data.
Spirometry and Impulse Oscillometry Infographic
 libterm.com
libterm.com