Dromotropic refers to the effect of a substance on the conduction velocity of the heart's electrical impulses, particularly through the atrioventricular node. Positive dromotropic agents increase conduction speed, while negative agents slow it down, impacting heart rhythm and overall cardiac function. Discover how dromotropic effects influence your heart health and why they matter in this detailed article.
Table of Comparison
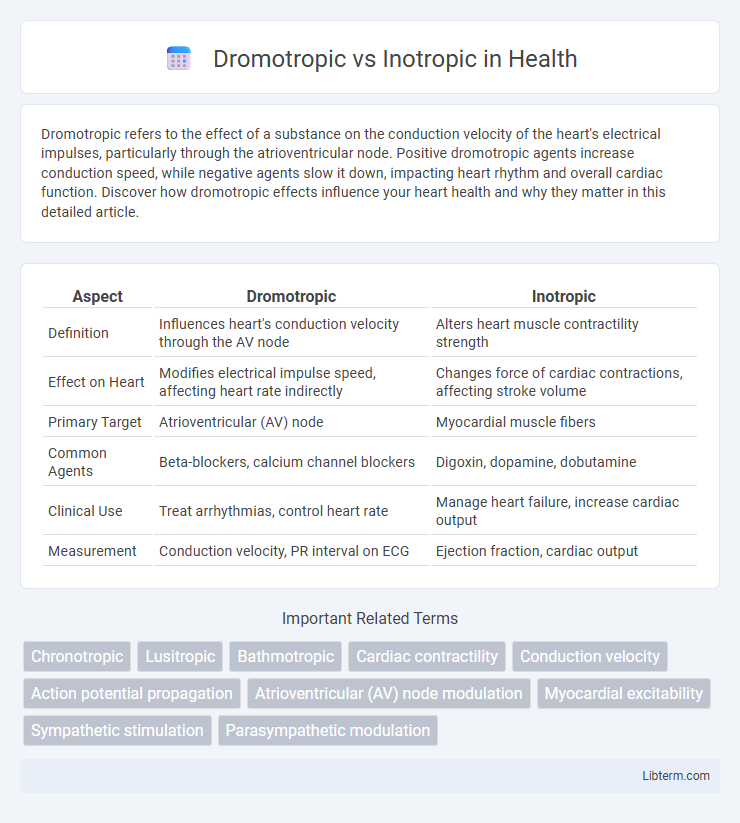
| Aspect | Dromotropic | Inotropic |
|---|---|---|
| Definition | Influences heart's conduction velocity through the AV node | Alters heart muscle contractility strength |
| Effect on Heart | Modifies electrical impulse speed, affecting heart rate indirectly | Changes force of cardiac contractions, affecting stroke volume |
| Primary Target | Atrioventricular (AV) node | Myocardial muscle fibers |
| Common Agents | Beta-blockers, calcium channel blockers | Digoxin, dopamine, dobutamine |
| Clinical Use | Treat arrhythmias, control heart rate | Manage heart failure, increase cardiac output |
| Measurement | Conduction velocity, PR interval on ECG | Ejection fraction, cardiac output |
Introduction to Cardiac Physiology
Dromotropic effects refer to changes in the conduction velocity of electrical impulses through the heart, primarily influencing the atrioventricular (AV) node, while inotropic effects pertain to alterations in myocardial contractility and the strength of heart muscle contractions. Cardiac physiology relies on these mechanisms to regulate heart rate and stroke volume, ensuring efficient blood circulation. Understanding dromotropic and inotropic influences is essential for managing conditions like heart failure and arrhythmias through targeted pharmacological interventions.
Defining Dromotropic Effects
Dromotropic effects specifically refer to the regulation of the conduction velocity of electrical impulses through the heart's atrioventricular (AV) node, directly influencing heart rhythm and timing. Positive dromotropic agents increase conduction speed, helping to correct certain bradyarrhythmias, while negative dromotropic agents slow AV nodal conduction, useful in managing tachyarrhythmias. Understanding dromotropic effects is essential in cardiac electrophysiology for modulating heart rate and synchronizing atrial and ventricular contractions effectively.
Understanding Inotropic Effects
Inotropic effects refer to the influence on myocardial contractility, directly affecting the force of heart muscle contractions. Positive inotropic agents, such as digoxin or dobutamine, enhance cardiac output by increasing contractile strength, which is critical in managing heart failure and cardiogenic shock. Understanding inotropic mechanisms aids in optimizing therapeutic strategies for cardiovascular diseases by targeting calcium ion availability and myocardial cell signaling pathways.
Key Differences: Dromotropic vs Inotropic
Dromotropic effects refer to the influence on the conduction velocity of electrical impulses through the heart's atrioventricular node, directly impacting the heart rate by either accelerating or delaying signal transmission. Inotropic effects specifically alter the strength or force of myocardial contraction without necessarily changing the heart rate or conduction speed, crucial for enhancing cardiac output in conditions like heart failure. The key difference lies in dromotropic effects modifying electrical conduction velocity, while inotropic effects modulate cardiac muscle contractility, each playing a distinct role in cardiovascular physiology and therapeutic interventions.
Mechanisms of Action in the Heart
Dromotropic effects influence the conduction velocity of electrical impulses through the atrioventricular node by modulating ion channel activity, particularly affecting calcium and sodium ion influx. Inotropic effects modify the contractile strength of cardiac muscle by altering intracellular calcium availability, primarily through the regulation of calcium ion channels and the sarcoplasmic reticulum calcium pump. Both mechanisms are crucial for maintaining efficient cardiac output and adjusting heart function in response to physiological demands.
Clinical Significance of Dromotropic Agents
Dromotropic agents influence the conduction velocity of electrical impulses through the heart's atrioventricular node, crucial for managing arrhythmias and heart block conditions. Positive dromotropes, such as isoproterenol, enhance conduction speed, improving cardiac output in bradyarrhythmias. Negative dromotropes, including beta-blockers and calcium channel blockers, slow conduction to prevent tachyarrhythmias and maintain hemodynamic stability.
Clinical Applications of Inotropic Agents
Inotropic agents primarily enhance myocardial contractility, making them vital in managing heart failure and cardiogenic shock where impaired cardiac output requires immediate support. Positive inotropes like dobutamine and milrinone increase stroke volume and cardiac output by augmenting calcium availability in cardiac cells, thereby improving tissue perfusion. These agents are essential in acute settings to stabilize patients with reduced ejection fraction, while ongoing clinical trials assess long-term outcomes and safety profiles.
Medications Influencing Dromotropic and Inotropic Effects
Medications influencing dromotropic effects primarily modulate the conduction velocity through the atrioventricular (AV) node, with negative dromotropic agents such as beta-blockers and calcium channel blockers slowing AV nodal conduction to treat arrhythmias. Inotropic agents alter myocardial contractility; positive inotropes like digoxin, dopamine, and dobutamine enhance cardiac output by increasing contractile strength, while negative inotropes such as beta-blockers reduce myocardial oxygen demand. Understanding the distinct pharmacodynamics of dromotropic and inotropic drugs is crucial for managing cardiac conditions like heart failure and supraventricular tachycardia.
Diagnostic Considerations in Cardiac Therapy
Dromotropic effects refer to the modulation of conduction velocity through the atrioventricular node, crucial for diagnosing arrhythmias and guiding cardiac therapy adjustments. Inotropic effects impact myocardial contractility, serving as key diagnostic indicators in heart failure evaluation and treatment optimization. Accurate assessment of dromotropic and inotropic responses through electrocardiography and echocardiography informs targeted therapeutic strategies to improve cardiac function.
Summary: Choosing the Right Cardiac Modulator
Dromotropic agents influence the conduction speed of electrical impulses through the heart's atrioventricular node, essential for managing arrhythmias. Inotropic agents directly affect myocardial contractility, critical for improving cardiac output in heart failure patients. Selecting the appropriate modulator depends on the patient's specific cardiac condition, targeting either electrical conduction or contractile strength for optimal therapeutic outcomes.
Dromotropic Infographic
 libterm.com
libterm.com