A brain abscess is a localized infection in the brain tissue that causes a collection of pus and swelling, often resulting from bacteria or fungi entering through a head injury, infection, or surgery. Symptoms may include headaches, fever, neurological deficits, and seizures, requiring prompt diagnosis via imaging like MRI or CT scans. Explore the rest of the article to understand the causes, symptoms, diagnosis, and treatment options for managing a brain abscess effectively.
Table of Comparison
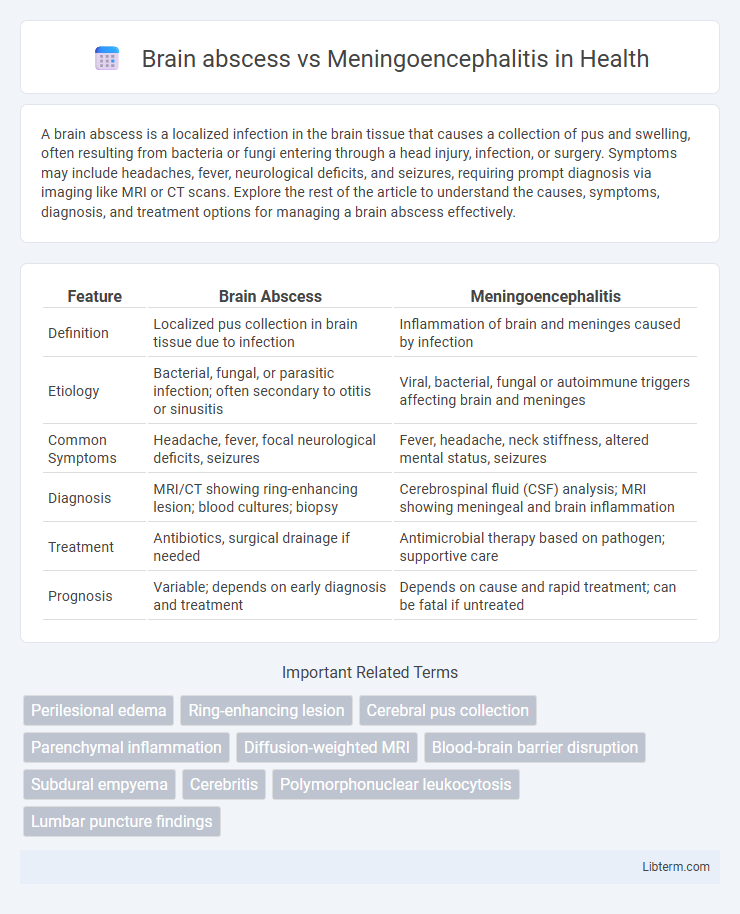
| Feature | Brain Abscess | Meningoencephalitis |
|---|---|---|
| Definition | Localized pus collection in brain tissue due to infection | Inflammation of brain and meninges caused by infection |
| Etiology | Bacterial, fungal, or parasitic infection; often secondary to otitis or sinusitis | Viral, bacterial, fungal or autoimmune triggers affecting brain and meninges |
| Common Symptoms | Headache, fever, focal neurological deficits, seizures | Fever, headache, neck stiffness, altered mental status, seizures |
| Diagnosis | MRI/CT showing ring-enhancing lesion; blood cultures; biopsy | Cerebrospinal fluid (CSF) analysis; MRI showing meningeal and brain inflammation |
| Treatment | Antibiotics, surgical drainage if needed | Antimicrobial therapy based on pathogen; supportive care |
| Prognosis | Variable; depends on early diagnosis and treatment | Depends on cause and rapid treatment; can be fatal if untreated |
Introduction to Brain Abscess and Meningoencephalitis
Brain abscess is a localized infection within the brain parenchyma, characterized by a collection of pus, inflammatory cells, and necrotic tissue, often caused by bacterial or fungal pathogens. Meningoencephalitis involves simultaneous inflammation of the meninges and brain tissue, usually due to viral, bacterial, or autoimmune causes, leading to widespread neurological dysfunction. Both conditions present significant clinical challenges requiring prompt diagnosis and targeted antimicrobial therapy to prevent neurological sequelae.
Epidemiology and Risk Factors
Brain abscess incidence ranges from 0.3 to 1.3 cases per 100,000 people annually, often associated with immunocompromised states, head trauma, or contiguous infections like otitis media. Meningoencephalitis presents more frequently worldwide, especially in regions with high prevalence of viral or bacterial pathogens, and risk factors include immunodeficiency, age extremes, and exposure to endemic vectors or contaminated water. Both conditions show increased occurrence in patients with compromised immune systems, but brain abscess is more commonly linked to localized infections whereas meningoencephalitis is predominantly caused by systemic or vector-borne agents.
Etiology and Causative Pathogens
Brain abscess etiology primarily involves localized infection of brain tissue often resulting from contiguous spread of bacterial infections such as otitis media, sinusitis, or dental infections, with common causative pathogens including Streptococcus species, Staphylococcus aureus, and anaerobic bacteria. Meningoencephalitis, characterized by simultaneous inflammation of the brain and meninges, is typically caused by viral pathogens like herpes simplex virus, enteroviruses, and arboviruses, although bacterial agents such as Neisseria meningitidis and Streptococcus pneumoniae may also be implicated. Understanding these distinct etiological pathways and pathogen profiles is essential for accurate diagnosis and targeted antimicrobial therapy.
Pathophysiology: Differences and Similarities
Brain abscess involves a localized collection of pus within the brain parenchyma caused by bacterial or fungal infection, leading to focal necrosis and edema, while meningoencephalitis represents a diffuse inflammation of both the meninges and brain tissue triggered by viral, bacterial, or autoimmune processes. Both conditions disrupt the blood-brain barrier and induce an immune response, but brain abscesses typically form encapsulated lesions with mass effect, whereas meningoencephalitis causes widespread neuronal damage and cytotoxic edema without a well-defined mass. Shared pathophysiological features include microglial activation, cytokine release, and increased intracranial pressure, which contribute to neurological dysfunction and inflammatory damage.
Clinical Presentation and Key Symptoms
Brain abscess typically presents with localized neurological deficits, headache, fever, and signs of increased intracranial pressure such as nausea and vomiting, often accompanied by a progressive focal neurological impairment. Meningoencephalitis manifests with a combination of meningeal irritation symptoms like neck stiffness, photophobia, and headache, alongside encephalitic features including altered mental status, seizures, and diffuse neurological deficits. Fever is common to both conditions, but the presence of focal neurological signs favors brain abscess, whereas widespread cerebral dysfunction suggests meningoencephalitis.
Diagnostic Imaging and Laboratory Findings
Brain abscess typically appears on MRI as a ring-enhancing lesion with central necrosis and surrounding edema, while meningoencephalitis demonstrates diffuse brain swelling and leptomeningeal enhancement. Laboratory analysis of brain abscess often reveals elevated white blood cell count in cerebrospinal fluid (CSF) with positive culture for causative bacteria, whereas meningoencephalitis presents with CSF pleocytosis, elevated protein, and either viral or bacterial identification by PCR or culture. Differentiating these conditions through imaging and CSF analysis is critical for appropriate antimicrobial therapy and surgical intervention.
Differential Diagnosis: Brain Abscess vs Meningoencephalitis
Differential diagnosis between brain abscess and meningoencephalitis centers on clinical presentation, imaging findings, and laboratory results. Brain abscess typically manifests as a focal lesion with ring-enhancing characteristics on MRI or CT, accompanied by localized neurological deficits and elevated intracranial pressure, whereas meningoencephalitis shows diffuse brain inflammation, often presenting with fever, headache, altered mental status, and diffuse white matter changes on imaging. Cerebrospinal fluid analysis reveals purulent fluid with elevated protein and neutrophilic predominance in brain abscess, while meningoencephalitis often has lymphocytic pleocytosis with variable protein and glucose levels, aiding in precise diagnosis and management.
Treatment Strategies and Management Approaches
Brain abscess treatment involves prompt surgical intervention through aspiration or excision combined with prolonged intravenous antibiotic therapy tailored to the causative organisms, often including metronidazole and third-generation cephalosporins. Management of meningoencephalitis emphasizes early administration of empirical antiviral agents such as acyclovir, alongside broad-spectrum antibiotics in suspected bacterial cases, supported by corticosteroids to reduce inflammatory responses in selected patients. Both conditions require close neurological monitoring, supportive care in intensive settings, and adjustment of therapy based on microbiological results and imaging follow-up.
Prognosis and Complications
Brain abscess prognosis depends on early diagnosis and effective surgical drainage combined with targeted antibiotics, with potential complications including increased intracranial pressure, seizures, and neurological deficits. Meningoencephalitis prognosis varies based on the causative pathogen and timeliness of antiviral or antibiotic treatment, while complications often involve cognitive impairment, persistent seizures, and brain edema. Both conditions require prompt intervention to minimize risks of long-term neurological damage and mortality.
Prevention and Patient Education
Effective prevention of brain abscess involves timely treatment of local infections such as sinusitis, otitis media, and dental infections, along with maintaining strong immune function, especially in immunocompromised patients. Prevention of meningoencephalitis centers on vaccination against causative pathogens like Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b, as well as practicing proper hygiene and avoiding exposure to infectious agents. Patient education should emphasize recognizing early symptoms, adherence to vaccination schedules, and seeking prompt medical care for infections to minimize the risk of these severe central nervous system infections.
Brain abscess Infographic
 libterm.com
libterm.com