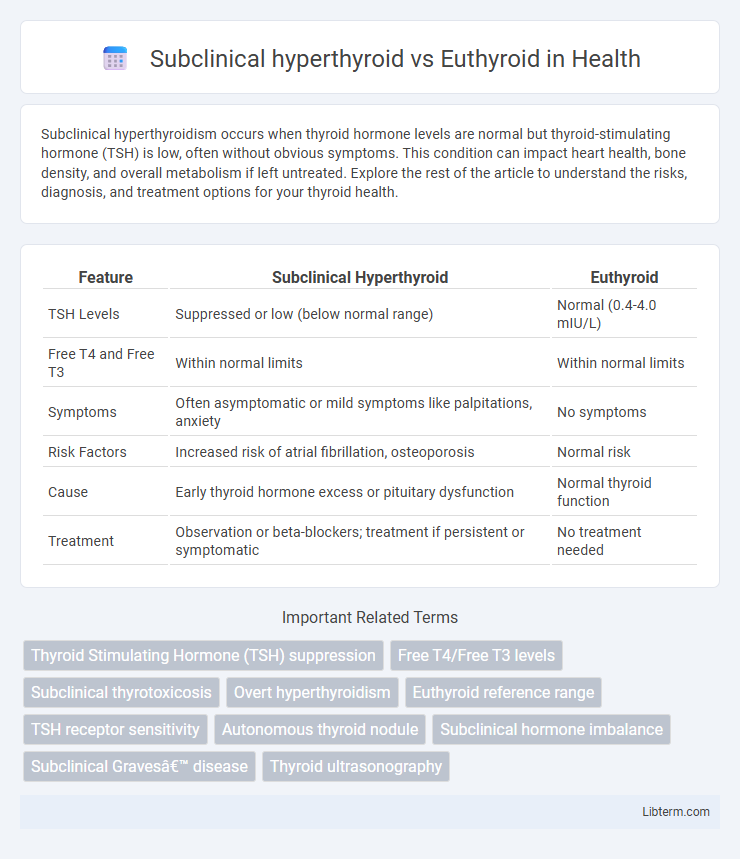
Subclinical hyperthyroidism occurs when thyroid hormone levels are normal but thyroid-stimulating hormone (TSH) is low, often without obvious symptoms. This condition can impact heart health, bone density, and overall metabolism if left untreated. Explore the rest of the article to understand the risks, diagnosis, and treatment options for your thyroid health.
Table of Comparison
| Feature | Subclinical Hyperthyroid | Euthyroid |
|---|---|---|
| TSH Levels | Suppressed or low (below normal range) | Normal (0.4-4.0 mIU/L) |
| Free T4 and Free T3 | Within normal limits | Within normal limits |
| Symptoms | Often asymptomatic or mild symptoms like palpitations, anxiety | No symptoms |
| Risk Factors | Increased risk of atrial fibrillation, osteoporosis | Normal risk |
| Cause | Early thyroid hormone excess or pituitary dysfunction | Normal thyroid function |
| Treatment | Observation or beta-blockers; treatment if persistent or symptomatic | No treatment needed |
Introduction to Thyroid Function
Thyroid function is regulated by the hypothalamic-pituitary-thyroid axis, controlling the secretion of thyroid hormones T3 and T4, which influence metabolism, growth, and energy balance. Subclinical hyperthyroidism is characterized by suppressed thyroid-stimulating hormone (TSH) levels with normal free T3 and T4 concentrations, indicating altered feedback without overt hormone excess. In contrast, euthyroid status reflects normal TSH and thyroid hormone levels, representing balanced thyroid function without signs of thyroid dysfunction.
Defining Subclinical Hyperthyroidism
Subclinical hyperthyroidism is characterized by low or undetectable serum thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) and free triiodothyronine (FT3) concentrations, distinguishing it from euthyroid status where TSH, FT4, and FT3 values all remain within normal reference ranges. This asymptomatic biochemical profile indicates altered hypothalamic-pituitary-thyroid axis regulation without overt signs of thyroid hormone excess. Subclinical hyperthyroidism can be transient or persistent and requires monitoring due to risks of atrial fibrillation, osteoporosis, and progression to overt hyperthyroidism.
Understanding Euthyroid State
The euthyroid state is characterized by thyroid hormone levels within normal reference ranges, ensuring optimal metabolic function and homeostasis. Unlike subclinical hyperthyroidism, where suppressed thyroid-stimulating hormone (TSH) levels occur despite normal free thyroxine (FT4) and triiodothyronine (T3) concentrations, euthyroid individuals maintain stable TSH signaling for proper endocrine balance. Understanding euthyroidism is essential for differentiating normal thyroid function from subtle thyroid dysfunctions that may impact cardiovascular health, bone density, and neurocognitive performance.
Key Differences in Hormone Levels
Subclinical hyperthyroidism is characterized by suppressed thyroid-stimulating hormone (TSH) levels below the normal reference range, typically under 0.4 mIU/L, while free thyroxine (FT4) and free triiodothyronine (FT3) levels remain within normal limits. Euthyroid individuals exhibit normal TSH, FT4, and FT3 concentrations, reflecting balanced thyroid function. The key difference lies in the low TSH in subclinical hyperthyroid states despite normal peripheral thyroid hormone levels.
Causes of Subclinical Hyperthyroidism
Subclinical hyperthyroidism is primarily caused by endogenous factors such as multinodular goiter, autonomous thyroid nodules, and Graves' disease in its early stages. Exogenous causes include excessive intake of thyroid hormone replacement therapy or iodine exposure. These conditions lead to suppressed TSH levels while maintaining normal free T4 and T3 concentrations, distinguishing subclinical hyperthyroidism from the euthyroid state.
Symptoms: Subclinical Hyperthyroid vs Euthyroid
Subclinical hyperthyroid individuals often experience subtle symptoms such as mild anxiety, palpitations, and heat intolerance that are typically absent in euthyroid patients. Euthyroid individuals maintain normal thyroid hormone levels, resulting in a stable metabolic state without symptoms like fatigue or weight changes seen in subclinical hyperthyroidism. Monitoring thyroid-stimulating hormone (TSH) levels is crucial for distinguishing subclinical hyperthyroidism from the asymptomatic euthyroid condition.
Diagnostic Criteria and Laboratory Evaluation
Subclinical hyperthyroidism is characterized by suppressed serum thyroid-stimulating hormone (TSH) levels below the normal reference range, typically <0.4 mIU/L, while free thyroxine (FT4) and free triiodothyronine (FT3) remain within normal limits, contrasting with euthyroid status where TSH, FT4, and FT3 levels all fall within established reference ranges. Laboratory evaluation relies on sensitive immunoassays measuring serum TSH as the most sensitive indicator, supported by concurrent FT4 and FT3 quantification to exclude overt hyperthyroidism. Establishing subclinical hyperthyroidism requires repeated testing to confirm persistently low TSH without clinical symptoms or biochemical evidence of thyroid hormone excess, distinguishing it from euthyroid individuals.
Potential Risks and Complications
Subclinical hyperthyroidism is associated with increased risks of atrial fibrillation, bone loss, and cardiovascular complications compared to euthyroid individuals with normal thyroid function. Patients with subclinical hyperthyroidism exhibit subtle thyroid hormone imbalances that may accelerate osteoporosis and heighten stroke risk in elderly populations. Careful monitoring and early intervention are critical to mitigate these potential complications and improve long-term outcomes.
Management and Treatment Approaches
Management of subclinical hyperthyroid typically involves careful monitoring of thyroid function tests and assessing cardiovascular risk, especially in patients over 65 or with osteoporosis. Treatment approaches may include low-dose antithyroid medications or radioactive iodine for persistent or symptomatic cases, while euthyroid individuals require no active intervention beyond routine health maintenance. Emphasis on individualized care plans ensures prevention of progression to overt hyperthyroidism and associated complications.
Prognosis and Long-Term Outcomes
Subclinical hyperthyroidism is associated with an increased risk of atrial fibrillation, cardiovascular morbidity, and osteoporosis compared to euthyroid individuals. Long-term outcomes often include progression to overt hyperthyroidism and potential cardiovascular complications, whereas euthyroid patients typically maintain stable thyroid function with minimal risk of these adverse events. Prognosis in subclinical hyperthyroidism depends on factors such as age, TSH levels, and underlying etiology, influencing management strategies and monitoring frequency.
Subclinical hyperthyroid Infographic
 libterm.com
libterm.com