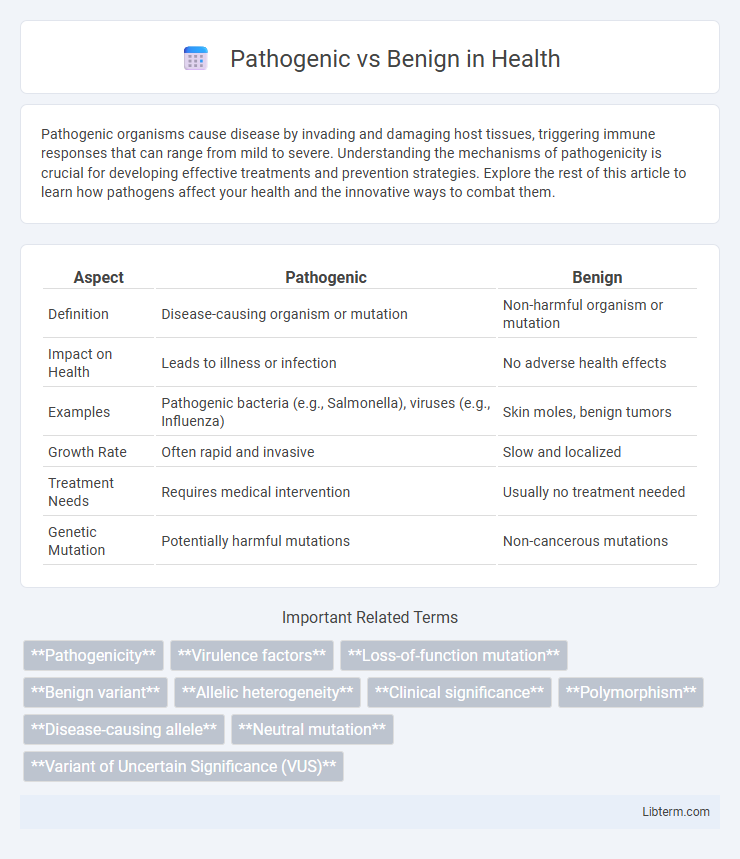
Pathogenic organisms cause disease by invading and damaging host tissues, triggering immune responses that can range from mild to severe. Understanding the mechanisms of pathogenicity is crucial for developing effective treatments and prevention strategies. Explore the rest of this article to learn how pathogens affect your health and the innovative ways to combat them.
Table of Comparison
| Aspect | Pathogenic | Benign |
|---|---|---|
| Definition | Disease-causing organism or mutation | Non-harmful organism or mutation |
| Impact on Health | Leads to illness or infection | No adverse health effects |
| Examples | Pathogenic bacteria (e.g., Salmonella), viruses (e.g., Influenza) | Skin moles, benign tumors |
| Growth Rate | Often rapid and invasive | Slow and localized |
| Treatment Needs | Requires medical intervention | Usually no treatment needed |
| Genetic Mutation | Potentially harmful mutations | Non-cancerous mutations |
Introduction to Pathogenic and Benign Entities
Pathogenic entities are microorganisms or agents that cause disease by invading host tissues, producing toxins, or disrupting normal physiological processes, leading to illness or infection. Benign entities, in contrast, are non-harmful organisms or conditions that do not cause disease and often coexist harmlessly within the host environment. Understanding the distinction between pathogenic and benign entities is crucial for accurate diagnosis, effective treatment, and the development of preventive healthcare strategies.
Defining Pathogenic vs Benign
Pathogenic refers to genetic variants or organisms that cause disease or harmful effects in a host, often linked to medical conditions requiring treatment. Benign denotes variants or entities that have no harmful impact and do not cause disease, typically considered harmless or neutral. Distinguishing pathogenic from benign is crucial for accurate diagnosis, risk assessment, and development of targeted therapies in clinical genetics.
Key Differences in Pathogenesis
Pathogenic microorganisms cause disease by invading host tissues, evading the immune response, and producing toxins, leading to cellular damage and inflammation. Benign organisms coexist without causing harm, often maintaining normal flora balance and supporting immune function. The key difference in pathogenesis lies in the pathogenic microbes' ability to disrupt homeostasis through virulence factors, while benign microbes lack these harmful mechanisms.
Mechanisms of Pathogenicity
Pathogenic organisms cause disease by producing toxins, invading host tissues, and evading the immune system through mechanisms such as secretion systems, adhesins, and immune modulation. In contrast, benign microbes lack these virulence factors and coexist with the host without causing damage or triggering a harmful immune response. Understanding these mechanisms is crucial for developing targeted antimicrobial therapies and diagnostic tools.
Characteristics of Benign Organisms
Benign organisms typically exhibit non-invasive growth patterns, limited replication rates, and do not produce toxins harmful to the host. Their cellular structures often lack virulence factors such as adhesins, enzymes, or capsules that facilitate pathogenicity. These organisms coexist with the host without causing tissue damage or eliciting significant immune responses, maintaining a symbiotic or commensal relationship.
Clinical Implications: Pathogenic vs Benign
Pathogenic variants directly contribute to disease development, necessitating targeted medical intervention and close monitoring to manage associated health risks effectively. Benign variants, however, do not cause disease and typically require no clinical treatment, serving mainly as reference points in genetic analysis. Differentiating between pathogenic and benign mutations is crucial for accurate diagnosis, personalized treatment plans, and informed genetic counseling.
Diagnostic Approaches and Challenges
Diagnostic approaches for distinguishing pathogenic from benign variants rely heavily on genomic sequencing technologies, including whole-exome sequencing and targeted gene panels, combined with bioinformatic tools that assess variant pathogenicity based on allele frequency, evolutionary conservation, and functional impact predictions. Challenges include variant interpretation complexity due to incomplete penetrance, variable expressivity, and the presence of variants of uncertain significance (VUS), which complicate clinical decision-making and require integration of phenotypic data, family history, and functional assays. Emerging approaches like machine learning algorithms and multi-omics integration aim to improve accuracy in variant classification, addressing limitations in current diagnostic frameworks.
Examples of Pathogenic and Benign Microbes
Pathogenic microbes such as Escherichia coli O157:H7, Mycobacterium tuberculosis, and Staphylococcus aureus cause diseases ranging from food poisoning to tuberculosis and skin infections. Benign microbes like Lactobacillus species in the gut microbiome, Saccharomyces cerevisiae used in baking, and Streptococcus thermophilus involved in yogurt production contribute to digestion, fermentation, and overall health without causing harm. Understanding the distinction between pathogenic and benign microbes is critical for developing targeted treatments and promoting beneficial microbial applications.
Immune Response to Pathogenic vs Benign Agents
The immune response to pathogenic agents involves activation of innate and adaptive immunity, characterized by inflammation, cytokine release, and recruitment of immune cells to eliminate harmful microorganisms. In contrast, benign agents typically elicit tolerance or a controlled immune response, preventing unnecessary tissue damage and maintaining homeostasis. This differential immune activation ensures effective defense against pathogens while minimizing chronic inflammation caused by harmless entities.
Prevention and Management Strategies
Pathogenic conditions require early detection and targeted treatment strategies to prevent progression and complications, including antimicrobial therapy and lifestyle modifications tailored to the specific pathogen. Benign conditions often benefit from regular monitoring and non-invasive interventions, emphasizing symptom management and preventative care to reduce the risk of escalation. Effective prevention and management hinge on accurate diagnosis, patient education, and adherence to individualized care plans to optimize health outcomes.
Pathogenic Infographic
 libterm.com
libterm.com