Monocytic cells play a crucial role in the immune system by differentiating into macrophages and dendritic cells that help fight infections and clear cellular debris. These cells are vital for inflammation response, tissue repair, and pathogen recognition. Explore the full article to understand how your body's monocytic function supports overall health and immune defense.
Table of Comparison
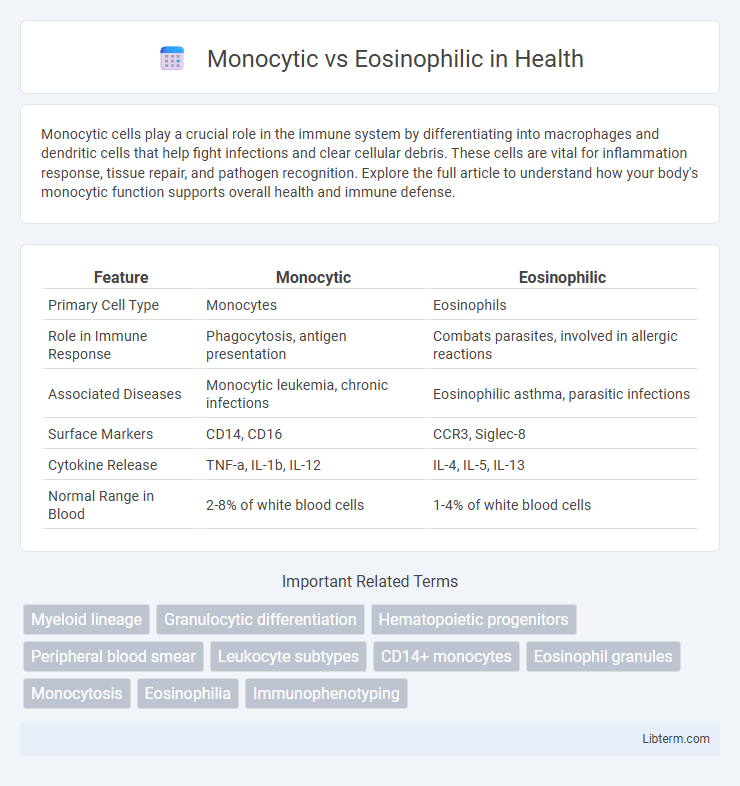
| Feature | Monocytic | Eosinophilic |
|---|---|---|
| Primary Cell Type | Monocytes | Eosinophils |
| Role in Immune Response | Phagocytosis, antigen presentation | Combats parasites, involved in allergic reactions |
| Associated Diseases | Monocytic leukemia, chronic infections | Eosinophilic asthma, parasitic infections |
| Surface Markers | CD14, CD16 | CCR3, Siglec-8 |
| Cytokine Release | TNF-a, IL-1b, IL-12 | IL-4, IL-5, IL-13 |
| Normal Range in Blood | 2-8% of white blood cells | 1-4% of white blood cells |
Introduction to Monocytic and Eosinophilic Cells
Monocytic cells, primarily monocytes, are a type of white blood cell involved in phagocytosis and immune response regulation, essential for fighting infections and inflammation. Eosinophilic cells, mainly eosinophils, play a critical role in combating parasitic infections and mediating allergic reactions through the release of cytotoxic granules. Understanding the distinct functions and mechanisms of monocytic and eosinophilic cells is crucial for diagnosing and treating various immune-related disorders.
Origin and Development: Monocytes vs Eosinophils
Monocytes originate from the myeloid progenitor cells in the bone marrow and mature into large phagocytic cells that circulate in the bloodstream before differentiating into macrophages or dendritic cells in tissues. Eosinophils also derive from myeloid progenitors but undergo a distinct developmental pathway influenced by interleukin-5 (IL-5), promoting their maturation into granulocytes specialized in combating parasitic infections and mediating allergic responses. Both cell types share a common myeloid lineage but differ significantly in their maturation signals, morphology, and immune functions.
Morphological Differences
Monocytic cells display large, kidney-shaped or indented nuclei with abundant gray-blue cytoplasm often containing fine granules, whereas eosinophilic cells feature bilobed nuclei and cytoplasm filled with prominent, coarse, reddish-orange granules. Monocytes are characterized by their irregular nuclear contours and lack of specific granules, aiding in phagocytic functions, while eosinophils contain distinctive eosin-staining granules involved in allergic responses and parasite defense. Morphological distinctions such as nucleus shape and granule presence are critical for differentiating these leukocytes in peripheral blood smears and bone marrow examinations.
Core Functions in Immune Response
Monocytic cells play a central role in phagocytosis and antigen presentation, crucial for initiating adaptive immune responses. Eosinophilic cells specialize in combating parasitic infections and modulating allergic inflammation through the release of cytotoxic granules and inflammatory mediators. Both cell types coordinate to maintain immune homeostasis and protect against diverse pathogens.
Role in Inflammatory Processes
Monocytic cells play a critical role in inflammatory processes by differentiating into macrophages and dendritic cells that phagocytize pathogens and release pro-inflammatory cytokines like TNF-alpha and IL-1. Eosinophilic cells contribute to inflammation primarily in allergic reactions and parasitic infections by releasing granule proteins such as major basic protein and eosinophil peroxidase, which modulate tissue damage and immune responses. The distinct roles of monocytic and eosinophilic cells underscore their importance in both initiating and regulating different types of inflammatory pathways.
Involvement in Disease States
Monocytic cells play a critical role in chronic inflammatory diseases like tuberculosis and atherosclerosis due to their ability to differentiate into macrophages that engulf pathogens and dead cells. Eosinophilic cells contribute predominantly to allergic reactions and parasitic infections by releasing cytotoxic granules that damage pathogens and modulate inflammation. Elevated monocytic counts are often associated with chronic infections and autoimmune disorders, while increased eosinophils are markers of asthma, atopic dermatitis, and helminthic infestations.
Diagnostic Markers and Laboratory Identification
Monocytic and eosinophilic cells are differentiated in laboratory identification by their distinct morphological features and specific diagnostic markers such as CD14 and CD16 for monocytes, and CCR3 and eosinophil peroxidase (EPX) for eosinophils. Flow cytometry and immunohistochemistry techniques are commonly used to detect these markers, aiding precise classification in blood or tissue samples. Elevated monocytic counts often indicate chronic inflammatory or infectious conditions, whereas increased eosinophilic levels are typically associated with allergic reactions or parasitic infections.
Clinical Implications of Monocytosis and Eosinophilia
Monocytosis, characterized by elevated monocyte counts above 800 cells/uL, often indicates chronic inflammatory conditions such as tuberculosis, sarcoidosis, or hematologic malignancies like chronic myelomonocytic leukemia. Eosinophilia, defined as eosinophil levels exceeding 500 cells/uL, is commonly associated with allergic reactions, parasitic infections, and certain autoimmune disorders like eosinophilic granulomatosis with polyangiitis. Accurate differentiation between monocytosis and eosinophilia through complete blood count and flow cytometry guides targeted diagnostic evaluation and tailored therapeutic strategies.
Treatment Considerations and Management
Treatment considerations for monocytic and eosinophilic disorders emphasize targeted therapies based on the underlying pathophysiology. Monocytic conditions often require immunosuppressive agents or chemotherapy to control abnormal monocytic cell proliferation, while eosinophilic disorders benefit from corticosteroids and biologics like anti-IL-5 antibodies to reduce eosinophil-driven inflammation. Management strategies also include monitoring organ involvement and tailoring treatments to mitigate tissue damage and improve patient outcomes.
Future Directions in Research and Therapy
Monocytic and eosinophilic pathways represent distinct immune responses with emerging research focusing on targeted therapies for chronic inflammatory diseases. Future directions involve the development of monocytic-specific inhibitors and eosinophil-targeting biologics to enhance precision medicine in conditions like asthma and autoimmune disorders. Advancements in single-cell sequencing and biomarker identification are expected to drive personalized treatment strategies and improve clinical outcomes.
Monocytic Infographic
 libterm.com
libterm.com