Thrombocythemia is a rare blood disorder characterized by an excessive production of platelets, increasing the risk of clot formation and potentially leading to strokes or heart attacks. Hemophilia is a genetic bleeding disorder where the blood lacks sufficient clotting factors, causing prolonged bleeding and difficulty in wound healing. Discover how these contrasting conditions affect your health and what steps you can take by reading the rest of this article.
Table of Comparison
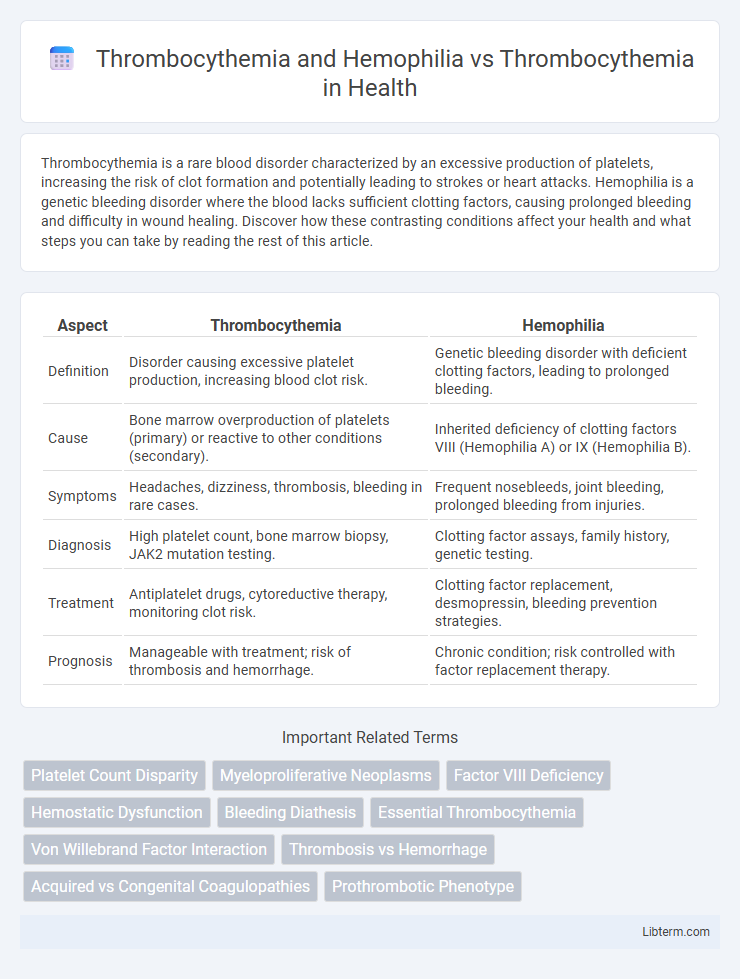
| Aspect | Thrombocythemia | Hemophilia |
|---|---|---|
| Definition | Disorder causing excessive platelet production, increasing blood clot risk. | Genetic bleeding disorder with deficient clotting factors, leading to prolonged bleeding. |
| Cause | Bone marrow overproduction of platelets (primary) or reactive to other conditions (secondary). | Inherited deficiency of clotting factors VIII (Hemophilia A) or IX (Hemophilia B). |
| Symptoms | Headaches, dizziness, thrombosis, bleeding in rare cases. | Frequent nosebleeds, joint bleeding, prolonged bleeding from injuries. |
| Diagnosis | High platelet count, bone marrow biopsy, JAK2 mutation testing. | Clotting factor assays, family history, genetic testing. |
| Treatment | Antiplatelet drugs, cytoreductive therapy, monitoring clot risk. | Clotting factor replacement, desmopressin, bleeding prevention strategies. |
| Prognosis | Manageable with treatment; risk of thrombosis and hemorrhage. | Chronic condition; risk controlled with factor replacement therapy. |
Understanding Thrombocythemia: Causes and Symptoms
Thrombocythemia is characterized by an abnormally high platelet count, often caused by genetic mutations such as JAK2, CALR, or MPL, leading to excessive blood clotting and increased risk of thrombosis. Hemophilia, in contrast, is a bleeding disorder caused by deficiencies in clotting factors VIII or IX, resulting in impaired blood clot formation despite normal platelet counts. Understanding the distinct etiologies and symptoms of thrombocythemia versus hemophilia is crucial for accurate diagnosis and targeted treatment.
What is Hemophilia? Key Features and Risks
Hemophilia is a genetic bleeding disorder characterized by the body's inability to form blood clots properly due to deficiencies in clotting factors VIII or IX, leading to prolonged bleeding and easy bruising. Key features include spontaneous bleeding episodes, especially into joints and muscles, and increased risk of severe hemorrhage after injuries or surgeries. Compared to thrombocythemia, which involves excessive platelet production causing clot formation, hemophilia presents a contrasting risk of uncontrolled bleeding rather than thrombosis.
Thrombocythemia vs. Hemophilia: Comparing Blood Disorders
Thrombocythemia is characterized by an abnormally high platelet count, leading to increased blood clotting risks, whereas hemophilia is a genetic disorder causing impaired blood clotting due to deficiencies in clotting factors VIII or IX. Unlike thrombocythemia, which often results in thrombosis and vascular complications, hemophilia primarily causes excessive bleeding and difficulty in stopping hemorrhages. Understanding these contrasting mechanisms is crucial for accurate diagnosis and targeted treatment of these distinct hematologic conditions.
Types of Thrombocythemia: Essential and Secondary
Thrombocythemia primarily manifests as Essential Thrombocythemia, a myeloproliferative disorder characterized by excessive platelet production without an obvious secondary cause, and Secondary Thrombocythemia, which results from underlying conditions such as inflammation, infection, or iron deficiency. Hemophilia differs fundamentally as a genetic bleeding disorder caused by deficiencies in clotting factors VIII or IX, leading to impaired blood coagulation. Understanding the distinction between Essential and Secondary Thrombocythemia is crucial for targeted diagnosis and treatment, contrasting with hemophilia's inherited coagulation deficiency.
Hemophilia: Types, Inheritance, and Diagnosis
Hemophilia is a genetic bleeding disorder characterized by deficient clotting factors, primarily hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency), both inherited in an X-linked recessive pattern affecting mostly males. Diagnosis involves coagulation tests including prolonged activated partial thromboplastin time (aPTT), factor assays to identify specific factor deficiency, and genetic testing to confirm mutations in F8 or F9 genes. Unlike thrombocythemia, which involves elevated platelet counts and risks thrombosis, hemophilia leads to excessive bleeding, requiring targeted clotting factor replacement and careful management to prevent hemorrhagic complications.
Blood Clotting Mechanisms in Thrombocythemia
Thrombocythemia is characterized by an excessive production of platelets, leading to heightened blood clotting risks through uncontrolled platelet aggregation and thrombus formation. Hemophilia, in contrast, is a genetic disorder marked by deficient clotting factors causing impaired blood clotting and excessive bleeding, despite normal or low platelet counts. The key distinction in blood clotting mechanisms lies in thrombocythemia's overactive platelet-driven thrombosis versus hemophilia's insufficient coagulation factor activity, highlighting divergent pathophysiological pathways affecting hemostasis.
Bleeding Risks: Hemophilia vs. the Thrombocythemic State
Hemophilia, a genetic disorder characterized by deficient clotting factors VIII or IX, results in severe bleeding risks due to impaired coagulation pathways. In contrast, thrombocythemia involves excessive platelet production, which paradoxically can cause both thrombotic complications and bleeding tendencies from dysfunctional platelets. While hemophilia primarily leads to spontaneous and prolonged bleeding episodes, bleeding in thrombocythemia is often related to platelet dysfunction despite high platelet counts, necessitating different therapeutic approaches.
Diagnosis: Laboratory Tests for Thrombocythemia and Hemophilia
Diagnosis of thrombocythemia involves complete blood count (CBC) showing elevated platelet levels often exceeding 450,000/uL, along with bone marrow biopsy revealing increased megakaryocytes. Hemophilia diagnosis primarily relies on coagulation tests such as prolonged activated partial thromboplastin time (aPTT) and factor VIII or IX assays for types A and B, respectively. Combining platelet function tests and genetic analysis aids differentiating thrombocythemia from hemophilia, as both affect hemostasis but present distinct laboratory profiles.
Treatment Approaches: Managing Thrombocythemia vs. Hemophilia
Treatment approaches for thrombocythemia focus on reducing platelet count through medications such as hydroxyurea or anagrelide and preventing clot formation with low-dose aspirin. Hemophilia management centers on replacing missing clotting factors through infusion therapies like factor VIII or IX concentrates to control bleeding episodes. While thrombocythemia treatment aims to prevent thrombosis, hemophilia therapy addresses bleeding risks by enhancing coagulation.
Prognosis and Quality of Life: Long-term Outcomes
Thrombocythemia generally presents a risk of thrombotic events but can be managed effectively with cytoreductive therapy, leading to a relatively favorable long-term prognosis and preserved quality of life. In contrast, patients with Hemophilia combined with Thrombocythemia face complex hemostatic challenges, increasing the risk of both bleeding and clotting complications that may worsen long-term outcomes and reduce quality of life. Tailored treatment strategies and regular monitoring are essential to improve survival rates and maintain functional status in these patients.
Thrombocythemia and Hemophilia Infographic
 libterm.com
libterm.com