Subarachnoid hemorrhage is a life-threatening condition caused by bleeding into the space surrounding the brain, often resulting from a ruptured aneurysm. Early recognition of symptoms such as sudden, severe headache, neck stiffness, and loss of consciousness is crucial for prompt medical intervention and improved outcomes. Explore the rest of the article to understand the causes, symptoms, diagnosis, and treatment options to protect your health.
Table of Comparison
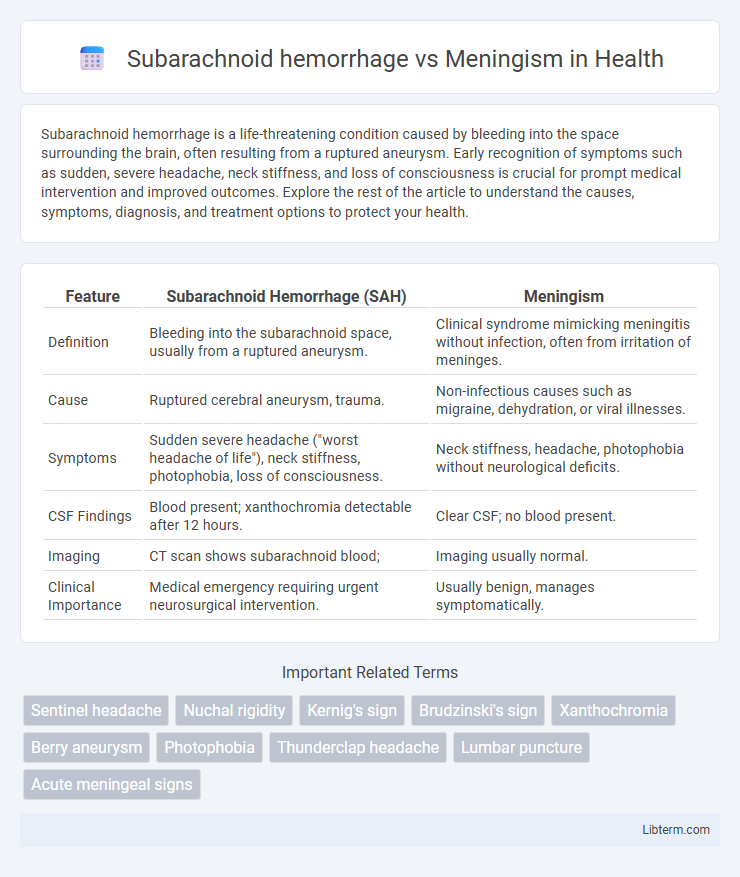
| Feature | Subarachnoid Hemorrhage (SAH) | Meningism |
|---|---|---|
| Definition | Bleeding into the subarachnoid space, usually from a ruptured aneurysm. | Clinical syndrome mimicking meningitis without infection, often from irritation of meninges. |
| Cause | Ruptured cerebral aneurysm, trauma. | Non-infectious causes such as migraine, dehydration, or viral illnesses. |
| Symptoms | Sudden severe headache ("worst headache of life"), neck stiffness, photophobia, loss of consciousness. | Neck stiffness, headache, photophobia without neurological deficits. |
| CSF Findings | Blood present; xanthochromia detectable after 12 hours. | Clear CSF; no blood present. |
| Imaging | CT scan shows subarachnoid blood; | Imaging usually normal. |
| Clinical Importance | Medical emergency requiring urgent neurosurgical intervention. | Usually benign, manages symptomatically. |
Introduction to Subarachnoid Hemorrhage and Meningism
Subarachnoid hemorrhage (SAH) is a critical condition characterized by bleeding into the subarachnoid space, often caused by ruptured cerebral aneurysms, leading to sudden severe headache, neck stiffness, and neurological deficits. Meningism presents with signs resembling meningitis such as neck stiffness, photophobia, and headache but lacks the infectious etiology, often caused by systemic illness or subarachnoid irritation. Differentiating SAH from meningism is vital due to the distinct pathophysiology and urgent need for neuroimaging and surgical intervention in SAH.
Definition and Overview
Subarachnoid hemorrhage (SAH) is a medical emergency characterized by bleeding into the subarachnoid space, often caused by ruptured cerebral aneurysms, leading to sudden severe headache, neurological deficits, and risk of complications like vasospasm. Meningism refers to a clinical syndrome with symptoms such as neck stiffness, photophobia, and headache, resembling meningitis but without actual infection or inflammation of the meninges. Differentiating SAH from meningism involves neuroimaging like CT scans to detect hemorrhage, whereas meningism typically results from non-infectious causes like migraine or cerebral irritation.
Etiology and Risk Factors
Subarachnoid hemorrhage (SAH) primarily results from the rupture of intracranial aneurysms or head trauma, with risk factors including hypertension, smoking, and genetic predisposition to vascular malformations. Meningism arises from meningeal irritation without infection, commonly triggered by migraine, subarachnoid hemorrhage, or other inflammatory processes affecting the meninges. Distinguishing these conditions relies on understanding that SAH involves bleeding in the subarachnoid space, whereas meningism represents a clinical syndrome characterized by neck stiffness and photophobia due to meningeal irritation.
Pathophysiology Comparison
Subarachnoid hemorrhage (SAH) results from bleeding into the subarachnoid space, typically due to aneurysmal rupture, causing increased intracranial pressure and irritation of the meninges. Meningism, by contrast, involves meningeal irritation without infection or bleeding, often triggered by inflammation, viral infections, or other non-hemorrhagic stimuli leading to symptoms like neck stiffness and photophobia. The key pathophysiological difference is that SAH causes direct blood-induced meningeal irritation and neurovascular compromise, whereas meningism arises from sterile inflammatory processes without hemorrhagic insult.
Clinical Presentation: Key Differences
Subarachnoid hemorrhage (SAH) typically presents with a sudden, severe "thunderclap" headache, often described as the worst headache of the patient's life, accompanied by nausea, vomiting, and possible loss of consciousness. Meningism presents with headache, neck stiffness, and photophobia, mimicking meningitis but without the infectious etiology or abnormal cerebrospinal fluid findings seen in SAH. Unlike meningism, SAH may show focal neurological deficits and signs of increased intracranial pressure on clinical examination and imaging.
Diagnostic Approach and Tools
Subarachnoid hemorrhage (SAH) diagnosis primarily relies on non-contrast computed tomography (CT) scans, which detect acute bleeding with high sensitivity within the first 72 hours of symptom onset, while lumbar puncture (LP) confirms xanthochromia if CT is negative but suspicion remains high. Meningism, characterized by meningeal irritation without infection or bleeding, requires clinical evaluation of symptoms such as neck stiffness, headache, and photophobia, alongside cerebrospinal fluid (CSF) analysis to exclude infectious causes or inflammatory conditions. Magnetic resonance imaging (MRI) and CSF cultures help differentiate meningism from intracranial hemorrhages and infectious meningitis, guiding appropriate management strategies.
Cerebrospinal Fluid Findings
Subarachnoid hemorrhage (SAH) typically presents with cerebrospinal fluid (CSF) showing xanthochromia and elevated red blood cells due to bleeding into the subarachnoid space. Meningism, related to irritation of the meninges without infection or hemorrhage, usually yields normal or mildly elevated white blood cells and no xanthochromia in CSF analysis. Differentiating SAH from meningism through lumbar puncture findings is critical for accurate diagnosis and timely management.
Imaging Studies: Role in Differentiation
Imaging studies play a crucial role in differentiating subarachnoid hemorrhage (SAH) from meningism by providing direct visualization of intracranial pathology. Non-contrast computed tomography (CT) scans demonstrate hyperdense blood in the subarachnoid space, a hallmark of SAH, often appearing within hours of symptom onset. In contrast, meningism, characterized by meningeal irritation without hemorrhage, typically shows normal CT imaging, necessitating cerebrospinal fluid analysis via lumbar puncture for definitive diagnosis.
Treatment Strategies and Management
Subarachnoid hemorrhage (SAH) treatment prioritizes rapid stabilization, blood pressure control, and surgical interventions such as aneurysm clipping or endovascular coiling to prevent rebleeding. In contrast, meningism, often presenting with meningeal irritation symptoms like neck stiffness and headache, is managed primarily through symptomatic relief, including analgesics and hydration, with no need for invasive neurosurgical procedures. Accurate diagnosis via neuroimaging and lumbar puncture guides the differentiation of SAH from meningism, ensuring appropriate management and improved patient outcomes.
Prognosis and Long-term Outcomes
Subarachnoid hemorrhage (SAH) often results in severe neurological deficits and has a high mortality rate, with long-term outcomes heavily influenced by the initial hemorrhage severity and timely intervention. Meningism typically presents with symptoms mimicking meningitis but lacks underlying infectious or hemorrhagic pathology, leading to a more favorable prognosis with full recovery expected. Prognostic evaluation for SAH includes monitoring for complications like vasospasm and hydrocephalus, which significantly impact long-term cognitive and functional outcomes.
Subarachnoid hemorrhage Infographic
 libterm.com
libterm.com