Leukocytosis is a condition characterized by an elevated white blood cell count, often signaling infection, inflammation, or other underlying health issues. Monitoring your white blood cell levels can provide critical insights into your immune system's response and help diagnose various medical conditions. Explore the rest of this article to understand the causes, symptoms, and treatment options for leukocytosis.
Table of Comparison
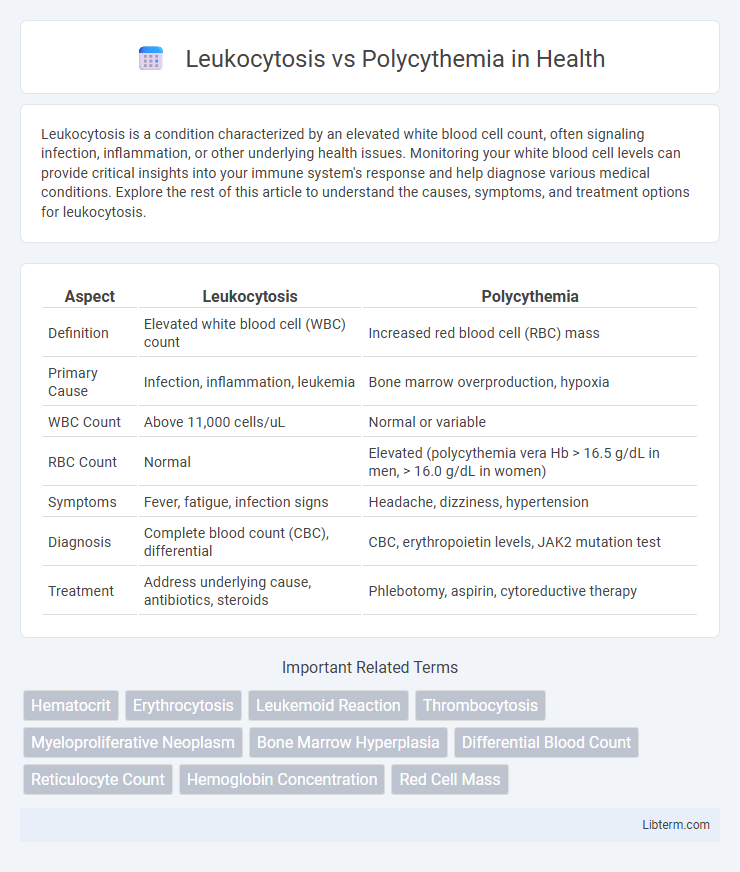
| Aspect | Leukocytosis | Polycythemia |
|---|---|---|
| Definition | Elevated white blood cell (WBC) count | Increased red blood cell (RBC) mass |
| Primary Cause | Infection, inflammation, leukemia | Bone marrow overproduction, hypoxia |
| WBC Count | Above 11,000 cells/uL | Normal or variable |
| RBC Count | Normal | Elevated (polycythemia vera Hb > 16.5 g/dL in men, > 16.0 g/dL in women) |
| Symptoms | Fever, fatigue, infection signs | Headache, dizziness, hypertension |
| Diagnosis | Complete blood count (CBC), differential | CBC, erythropoietin levels, JAK2 mutation test |
| Treatment | Address underlying cause, antibiotics, steroids | Phlebotomy, aspirin, cytoreductive therapy |
Introduction to Leukocytosis and Polycythemia
Leukocytosis is characterized by an elevated white blood cell count, often indicating infection, inflammation, or hematologic malignancies. Polycythemia involves an increased red blood cell mass, leading to heightened blood viscosity and potential complications like thrombosis. Both conditions require precise hematologic evaluation to determine underlying causes and appropriate management strategies.
Definition of Leukocytosis
Leukocytosis is a medical condition characterized by an elevated white blood cell (WBC) count above the normal range, typically exceeding 11,000 cells per microliter of blood. It serves as a response to infections, inflammation, stress, or bone marrow disorders, and is distinguished from polycythemia, which involves an increased red blood cell (RBC) count or hematocrit level. Diagnosing leukocytosis involves complete blood count (CBC) tests to identify the specific type and cause of the elevated leukocytes.
Definition of Polycythemia
Polycythemia is a hematologic condition characterized by an increased concentration of red blood cells in the bloodstream, resulting in elevated hematocrit and hemoglobin levels. Unlike leukocytosis, which involves an abnormal rise in white blood cells, polycythemia specifically affects erythrocyte production, often caused by bone marrow disorders or chronic hypoxia. This abnormal proliferation leads to increased blood viscosity, raising the risk of thrombosis and cardiovascular complications.
Key Differences Between Leukocytosis and Polycythemia
Leukocytosis is characterized by an elevated white blood cell count, typically indicating infection or inflammation, while polycythemia involves an increased red blood cell mass, often leading to thicker blood and higher risk of thrombosis. Leukocytosis primarily affects immune response mechanisms, whereas polycythemia impacts oxygen transport efficiency and blood viscosity. Laboratory tests distinguishing these conditions include complete blood count (CBC) with differential for leukocytosis and hematocrit or hemoglobin concentration for polycythemia diagnosis.
Causes of Leukocytosis
Leukocytosis primarily results from infections, inflammation, stress, tissue damage, or hematologic disorders such as leukemia, causing an elevated white blood cell count. Unlike polycythemia, which is characterized by increased red blood cell mass often due to chronic hypoxia or bone marrow disorders, leukocytosis reflects the body's immune response to various physiologic or pathological stimuli. Understanding the etiology of leukocytosis is crucial for differential diagnosis and appropriate management of underlying conditions.
Causes of Polycythemia
Polycythemia primarily results from increased red blood cell production due to chronic hypoxia, as seen in conditions like chronic obstructive pulmonary disease (COPD) and living at high altitudes, or from genetic mutations such as JAK2 V617F in polycythemia vera. Secondary polycythemia can also arise from erythropoietin-secreting tumors or renal artery stenosis stimulating excessive erythropoietin production. In contrast, leukocytosis involves elevated white blood cell counts typically caused by infection, inflammation, or hematologic malignancies.
Clinical Manifestations and Symptoms
Leukocytosis presents clinically with symptoms like fever, fatigue, and frequent infections due to elevated white blood cell counts. Polycythemia manifests through headaches, dizziness, and hypertension resulting from increased red blood cell mass and blood viscosity. Both conditions risk complications such as thrombosis but differ fundamentally in hematologic profiles and symptomatology.
Diagnostic Approaches
Leukocytosis diagnosis primarily involves a complete blood count (CBC) with differential to identify elevated white blood cell levels and potential underlying infections or hematologic disorders. Polycythemia diagnosis relies on measuring hematocrit and hemoglobin concentrations, alongside erythropoietin levels and arterial oxygen saturation, to distinguish between primary polycythemia vera and secondary causes. Bone marrow biopsy and genetic testing for JAK2 mutations are critical for confirming polycythemia vera, whereas leukocytosis may require additional tests to identify specific infectious or malignant sources.
Treatment and Management Strategies
Leukocytosis treatment primarily targets the underlying cause, such as infections or inflammation, with antibiotics, anti-inflammatory drugs, or corticosteroids, while severe cases may require chemotherapy or bone marrow suppression. Polycythemia management involves phlebotomy to reduce hematocrit levels and prevent blood clots, alongside low-dose aspirin therapy to reduce thrombosis risk. For polycythemia vera, cytoreductive therapy with hydroxyurea or interferon-alpha is used to control red blood cell production and minimize complications.
Prognosis and Long-term Outcomes
Leukocytosis prognosis varies widely depending on the underlying cause, with reactive leukocytosis often resolving after treating infections or inflammation, while chronic leukemias may require ongoing management and carry a variable long-term outlook. Polycythemia, particularly Polycythemia Vera, poses risks including thrombotic events and progression to myelofibrosis or acute leukemia, necessitating lifelong monitoring and therapeutic phlebotomy or cytoreductive therapy to improve survival. Both conditions demand early diagnosis and tailored treatment strategies to mitigate complications and optimize long-term patient outcomes.
Leukocytosis Infographic
 libterm.com
libterm.com