Fibrillation is a rapid, irregular heartbeat often linked to atrial or ventricular muscle dysfunction that can significantly impact heart efficiency. This condition may cause symptoms like palpitations, shortness of breath, and increased risk of stroke if left untreated. Discover essential insights and management strategies for fibrillation in the rest of this article to protect your heart health.
Table of Comparison
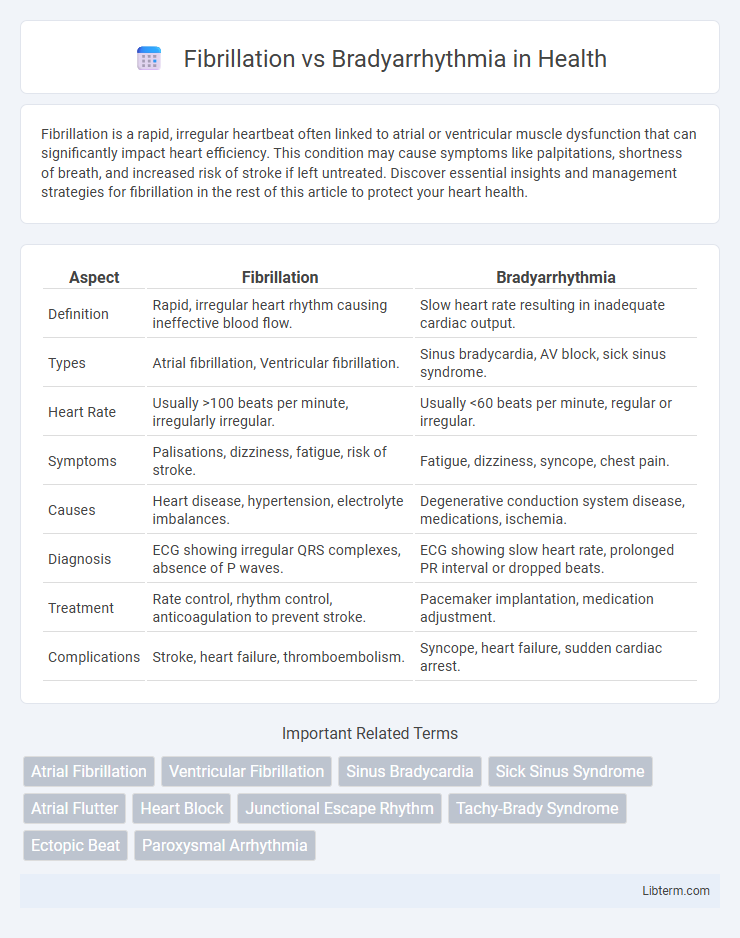
| Aspect | Fibrillation | Bradyarrhythmia |
|---|---|---|
| Definition | Rapid, irregular heart rhythm causing ineffective blood flow. | Slow heart rate resulting in inadequate cardiac output. |
| Types | Atrial fibrillation, Ventricular fibrillation. | Sinus bradycardia, AV block, sick sinus syndrome. |
| Heart Rate | Usually >100 beats per minute, irregularly irregular. | Usually <60 beats per minute, regular or irregular. |
| Symptoms | Palisations, dizziness, fatigue, risk of stroke. | Fatigue, dizziness, syncope, chest pain. |
| Causes | Heart disease, hypertension, electrolyte imbalances. | Degenerative conduction system disease, medications, ischemia. |
| Diagnosis | ECG showing irregular QRS complexes, absence of P waves. | ECG showing slow heart rate, prolonged PR interval or dropped beats. |
| Treatment | Rate control, rhythm control, anticoagulation to prevent stroke. | Pacemaker implantation, medication adjustment. |
| Complications | Stroke, heart failure, thromboembolism. | Syncope, heart failure, sudden cardiac arrest. |
Understanding Cardiac Arrhythmias
Fibrillation, characterized by rapid and irregular heartbeats, disrupts the coordinated contraction of the atria or ventricles, significantly increasing the risk of stroke and heart failure. Bradyarrhythmia involves abnormally slow heart rates due to impaired electrical signals in the sinoatrial node or atrioventricular conduction system, often leading to fatigue, dizziness, or syncope. Understanding these cardiac arrhythmias is crucial for accurate diagnosis and effective treatment, which may include medications, pacemaker implantation, or electrophysiological interventions.
What is Fibrillation?
Fibrillation refers to rapid, irregular electrical impulses in the heart's atria or ventricles, causing ineffective contraction and impaired blood flow. Atrial fibrillation is the most common type, leading to increased risk of stroke and heart failure. Unlike bradyarrhythmia, which involves abnormally slow heart rhythms, fibrillation results in chaotic, high-frequency electrical activity disrupting normal heart function.
Types of Fibrillation: Atrial vs Ventricular
Atrial fibrillation is the most common type of fibrillation characterized by rapid, irregular beating of the atria, often leading to stroke and heart failure if untreated. Ventricular fibrillation, a life-threatening condition, involves chaotic electrical activity in the ventricles causing sudden cardiac arrest without immediate intervention. Bradyarrhythmia involves slow heart rhythms due to impaired conduction, distinct from the rapid and erratic contractions seen in both atrial and ventricular fibrillation.
What is Bradyarrhythmia?
Bradyarrhythmia is a condition characterized by an abnormally slow heart rate, typically below 60 beats per minute, resulting from impaired electrical signals in the heart. This slow rhythm can cause symptoms such as dizziness, fatigue, and fainting due to insufficient blood flow to the body. Unlike fibrillation, which involves rapid and irregular heartbeats, bradyarrhythmia reflects a decreased heart rate that disrupts normal cardiac function.
Causes of Fibrillation
Fibrillation, characterized by rapid and irregular heartbeats, is primarily caused by electrical signal disruptions in the atria or ventricles, often triggered by conditions such as coronary artery disease, hypertension, cardiomyopathy, and electrolyte imbalances. Atrial fibrillation specifically arises from multiple re-entrant wavelets or focal ectopic activity, frequently linked to atrial dilation or fibrosis. In contrast, bradyarrhythmia involves abnormally slow heart rhythms caused mainly by sinoatrial node dysfunction or atrioventricular conduction block rather than these electrical disturbances typical of fibrillation.
Causes of Bradyarrhythmia
Bradyarrhythmia primarily results from impaired electrical conduction within the sinoatrial node or atrioventricular node, often caused by age-related degeneration, ischemic heart disease, or excessive vagal tone. Other significant causes include medication effects, such as beta-blockers and calcium channel blockers, and intrinsic conduction system diseases like sick sinus syndrome or heart block. Understanding these etiologies is critical for accurate diagnosis and effective management of bradyarrhythmia compared to fibrillation.
Symptoms: Fibrillation vs Bradyarrhythmia
Fibrillation presents symptoms such as rapid, irregular heartbeat, palpitations, dizziness, and shortness of breath, often leading to fatigue or chest discomfort. Bradyarrhythmia symptoms include slow heart rate, fatigue, lightheadedness, syncope, and sometimes confusion due to decreased cardiac output. Both conditions can severely impair cardiac efficiency, but fibrillation typically causes rapid and chaotic heart rhythms, while bradyarrhythmia results in abnormally slow rhythms.
Diagnostic Methods for Arrhythmias
Electrocardiography (ECG) is the primary diagnostic method for differentiating fibrillation, such as atrial fibrillation characterized by irregular, rapid heartbeats, from bradyarrhythmias, which involve abnormally slow heart rates often detected by prolonged PR intervals or pauses. Holter monitoring and event recorders provide continuous rhythm assessment, improving detection of intermittent arrhythmias by capturing transient fibrillation episodes or bradycardic events outside clinical settings. Advanced imaging techniques like electrophysiological studies offer detailed mapping of electrical conduction pathways, aiding precise diagnosis and guiding tailored therapeutic interventions for complex arrhythmias.
Treatment Options: Fibrillation and Bradyarrhythmia
Treatment options for fibrillation, such as atrial fibrillation, often include anticoagulants to reduce stroke risk, rate control medications like beta-blockers or calcium channel blockers, and rhythm control through antiarrhythmic drugs or catheter ablation. Bradyarrhythmia treatments focus on addressing the underlying cause, with pacemaker implantation being the primary option for symptomatic bradycardia to maintain adequate heart rate and cardiac output. Both conditions may require lifestyle modifications and continuous monitoring to optimize patient outcomes and prevent complications.
Prognosis and Complications
Fibrillation, particularly atrial fibrillation, carries a significant risk of stroke and heart failure due to chaotic atrial activity and ineffective blood flow, often requiring anticoagulation to prevent thromboembolism. Bradyarrhythmia, characterized by abnormally slow heart rates, can lead to syncope, fatigue, and in severe cases, sudden cardiac arrest if untreated, commonly managed with pacemaker implantation. The prognosis for fibrillation depends on stroke prevention and rate control, while bradyarrhythmia prognosis improves markedly after timely device therapy, though both conditions can significantly increase morbidity without proper management.
Fibrillation Infographic
 libterm.com
libterm.com