Hyponatremia occurs when your blood sodium levels drop below normal, leading to symptoms such as headache, confusion, and fatigue. This condition can result from various causes including excessive fluid intake, kidney problems, or certain medications. Explore the rest of the article to understand the causes, symptoms, and effective treatments for hyponatremia.
Table of Comparison
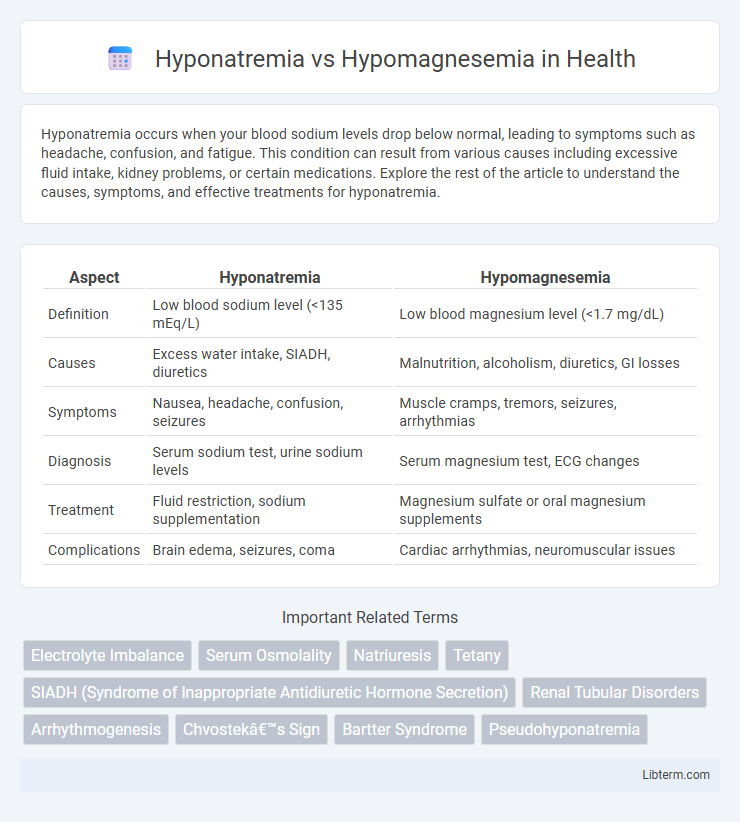
| Aspect | Hyponatremia | Hypomagnesemia |
|---|---|---|
| Definition | Low blood sodium level (<135 mEq/L) | Low blood magnesium level (<1.7 mg/dL) |
| Causes | Excess water intake, SIADH, diuretics | Malnutrition, alcoholism, diuretics, GI losses |
| Symptoms | Nausea, headache, confusion, seizures | Muscle cramps, tremors, seizures, arrhythmias |
| Diagnosis | Serum sodium test, urine sodium levels | Serum magnesium test, ECG changes |
| Treatment | Fluid restriction, sodium supplementation | Magnesium sulfate or oral magnesium supplements |
| Complications | Brain edema, seizures, coma | Cardiac arrhythmias, neuromuscular issues |
Introduction to Hyponatremia and Hypomagnesemia
Hyponatremia is a common electrolyte disorder characterized by low sodium levels in the blood, typically below 135 mEq/L, leading to symptoms such as headache, confusion, and seizures. Hypomagnesemia involves a deficiency of magnesium in the bloodstream, often defined by serum magnesium levels under 1.7 mg/dL, and results in neuromuscular irritability, arrhythmias, and metabolic disturbances. Both conditions affect critical physiological functions and require prompt diagnosis to prevent severe complications.
Definition and Etiology
Hyponatremia is defined as a serum sodium concentration below 135 mmol/L, resulting from excessive water retention or sodium loss, often caused by conditions such as heart failure, cirrhosis, or syndrome of inappropriate antidiuretic hormone secretion (SIADH). Hypomagnesemia refers to low serum magnesium levels under 1.7 mg/dL, frequently linked to gastrointestinal losses, chronic alcoholism, or use of diuretics and certain medications. Both electrolyte disturbances disrupt cellular function but differ in underlying mechanisms and clinical implications due to their distinct etiologies.
Prevalence and Risk Factors
Hyponatremia, characterized by low sodium levels in the blood, affects approximately 15-30% of hospitalized patients, with elderly individuals and those with heart failure, liver cirrhosis, or kidney disease at highest risk. Hypomagnesemia, marked by deficient magnesium levels, has a prevalence rate of around 12-15% in hospitalized patients, especially common among individuals with malnutrition, chronic alcoholism, or those on diuretics and proton pump inhibitors. Both electrolyte disturbances share risk factors such as gastrointestinal losses and certain medications, but hypomagnesemia often underpins refractory cases of hyponatremia due to its role in sodium and potassium balance.
Pathophysiological Mechanisms
Hyponatremia results from an imbalance in water and sodium regulation often caused by excessive water retention or sodium loss, leading to osmotic shifts and cellular edema. Hypomagnesemia arises due to impaired magnesium absorption, increased renal excretion, or redistribution, disrupting enzymatic processes and ion channel functions critical for neuromuscular and cardiovascular stability. Both electrolyte disturbances involve altered membrane potentials and cellular dysfunction but differ fundamentally in their underlying pathophysiological mechanisms and clinical implications.
Clinical Manifestations and Symptoms
Hyponatremia presents clinically with symptoms such as headache, nausea, confusion, seizures, and in severe cases, coma due to cerebral edema from low sodium levels. Hypomagnesemia manifests with neuromuscular irritability, including muscle cramps, tremors, tetany, and cardiac arrhythmias like torsades de pointes, often accompanied by hypokalemia and hypocalcemia. Both electrolyte imbalances require careful assessment of clinical signs for timely diagnosis and management to prevent complications.
Diagnostic Criteria and Laboratory Findings
Hyponatremia is characterized by serum sodium levels below 135 mEq/L, often diagnosed through serum electrolyte testing revealing low sodium and possible hypo-osmolality, whereas hypomagnesemia is defined by serum magnesium levels under 1.7 mg/dL, detected via serum magnesium assays. Diagnostic criteria for hyponatremia include assessing serum osmolality, urine sodium concentration, and volume status to differentiate between hypo-, eu-, and hypervolemic states, while hypomagnesemia diagnosis involves measuring total magnesium, with attention to ionized magnesium and concurrent electrolyte abnormalities such as hypokalemia or hypocalcemia. Laboratory findings for hyponatremia typically show low plasma sodium with varying urine sodium excretion, contrasted by hypomagnesemia laboratory results highlighting low serum magnesium and potential secondary findings like decreased parathyroid hormone or altered renal magnesium handling.
Differential Diagnosis
Hyponatremia is characterized by low serum sodium levels typically below 135 mEq/L, often presenting with symptoms such as confusion, seizures, and muscle cramps, whereas hypomagnesemia involves magnesium deficiency below 1.7 mg/dL, leading to neuromuscular irritability, tremors, and cardiac arrhythmias. Differential diagnosis requires evaluating electrolyte panels, renal function, and underlying causes like diuretics use, gastrointestinal losses, or endocrine disorders, with hyponatremia frequently linked to volume status changes and SIADH, while hypomagnesemia is often associated with malnutrition, alcoholism, or chronic diarrhea. Accurate diagnosis depends on correlating clinical findings with laboratory results, enabling targeted treatment of the specific electrolyte imbalance to prevent complications such as neurological impairment or cardiac dysrhythmias.
Management and Treatment Strategies
Management of hyponatremia involves careful correction of serum sodium levels through controlled administration of hypertonic saline in severe cases and fluid restriction in hypotonic hyponatremia, avoiding rapid shifts to prevent osmotic demyelination syndrome. Treatment of hypomagnesemia focuses on magnesium replacement, using oral magnesium supplements for mild cases and intravenous magnesium sulfate for severe or symptomatic deficiencies to restore normal magnesium levels and prevent cardiac arrhythmias, seizures, and neuromuscular irritability. Monitoring electrolyte levels and addressing underlying causes are critical in both conditions to ensure effective and safe correction.
Complications and Prognosis
Hyponatremia can lead to severe neurological complications, including confusion, seizures, and cerebral edema, with prognosis depending on the rate and severity of sodium imbalance. Hypomagnesemia often results in cardiac arrhythmias, neuromuscular irritability, and refractory electrolyte disturbances, significantly impacting morbidity if not promptly corrected. Both conditions require timely diagnosis and management to prevent long-term complications and improve patient outcomes.
Prevention and Patient Education
Preventing hyponatremia involves maintaining balanced sodium intake tailored to individual health conditions, avoiding excessive water consumption, and monitoring medications that can alter sodium levels such as diuretics. Patient education should emphasize recognizing early symptoms like nausea, headache, and confusion, alongside guidance to seek timely medical evaluation to adjust treatment plans accordingly. For hypomagnesemia, prevention centers on ensuring adequate dietary magnesium from sources like nuts, green leafy vegetables, and whole grains, and managing underlying causes like gastrointestinal losses or chronic alcoholism, while patient education focuses on understanding symptoms such as muscle cramps, seizures, and cardiac arrhythmias to promote prompt healthcare intervention.
Hyponatremia Infographic
 libterm.com
libterm.com