Functional heartburn is characterized by typical heartburn symptoms without any detectable acid reflux or esophageal motility disorders, often making diagnosis challenging. This condition can significantly impact your quality of life due to persistent discomfort despite normal test results and standard treatments. Explore the rest of this article to understand the causes, symptoms, and effective management strategies for functional heartburn.
Table of Comparison
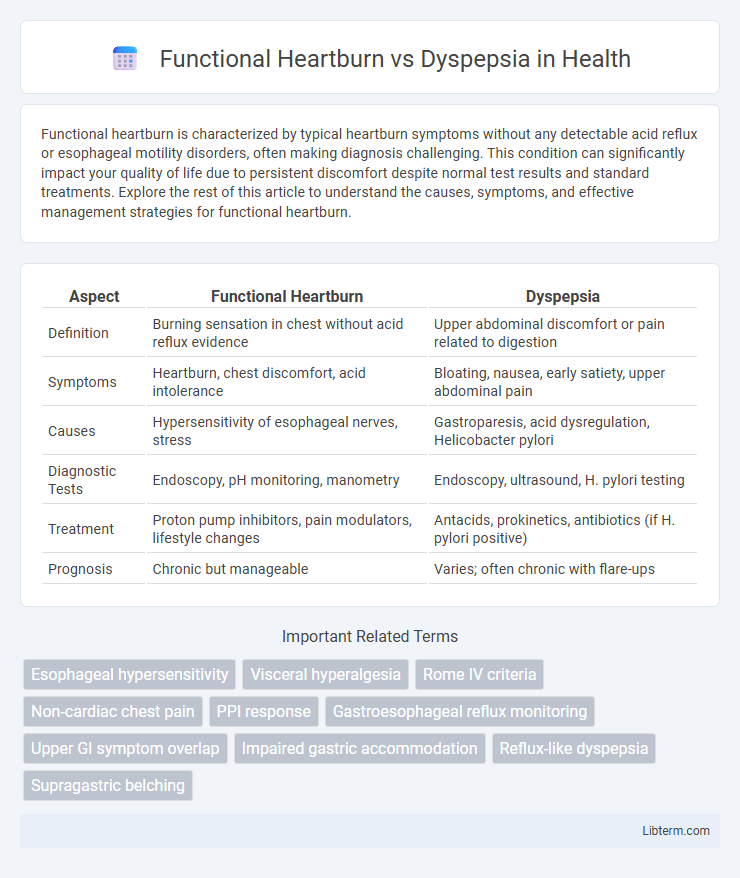
| Aspect | Functional Heartburn | Dyspepsia |
|---|---|---|
| Definition | Burning sensation in chest without acid reflux evidence | Upper abdominal discomfort or pain related to digestion |
| Symptoms | Heartburn, chest discomfort, acid intolerance | Bloating, nausea, early satiety, upper abdominal pain |
| Causes | Hypersensitivity of esophageal nerves, stress | Gastroparesis, acid dysregulation, Helicobacter pylori |
| Diagnostic Tests | Endoscopy, pH monitoring, manometry | Endoscopy, ultrasound, H. pylori testing |
| Treatment | Proton pump inhibitors, pain modulators, lifestyle changes | Antacids, prokinetics, antibiotics (if H. pylori positive) |
| Prognosis | Chronic but manageable | Varies; often chronic with flare-ups |
Understanding Functional Heartburn
Functional heartburn is characterized by persistent burning sensations in the chest without evidence of acid reflux or esophageal motility disorders, differentiating it from gastroesophageal conditions. Unlike dyspepsia, which primarily involves upper abdominal discomfort, bloating, and nausea related to digestive disturbances, functional heartburn centers on esophageal hypersensitivity and impaired pain perception. Diagnostic evaluation for functional heartburn includes endoscopy and pH monitoring to exclude gastroesophageal reflux disease (GERD), emphasizing its distinct pathophysiology and management strategies.
Defining Dyspepsia
Dyspepsia, commonly known as indigestion, refers to persistent or recurrent pain or discomfort centered in the upper abdomen, often accompanied by bloating, nausea, or early satiety. Unlike functional heartburn, which primarily involves a burning sensation behind the breastbone caused by acid reflux without visible esophageal damage, dyspepsia encompasses a broader range of gastrointestinal symptoms related to the stomach and upper digestive tract. Diagnostic criteria for dyspepsia typically exclude structural causes, focusing on functional disturbances affecting gastric motility or sensitivity.
Symptoms Comparison: Functional Heartburn vs Dyspepsia
Functional heartburn primarily presents with a burning sensation behind the breastbone, often unrelated to meals, whereas dyspepsia typically manifests as upper abdominal discomfort, bloating, and early satiety. Unlike dyspepsia, functional heartburn symptoms are not consistently linked to food intake or gastric motility issues. Both conditions may cause overlapping symptoms such as nausea and belching, but the localization and triggers of pain or discomfort differ significantly, aiding in differential diagnosis.
Causes and Risk Factors
Functional heartburn arises from hypersensitivity of the esophageal lining and impaired lower esophageal sphincter function, often triggered by acid reflux without visible tissue damage. Dyspepsia, or indigestion, typically results from delayed gastric emptying, Helicobacter pylori infection, and abnormal gastrointestinal motility affecting the upper digestive tract. Risk factors for functional heartburn include obesity, smoking, and stress, while dyspepsia is commonly associated with NSAID use, diet high in fatty foods, and psychosocial stressors.
Diagnostic Approaches
Diagnostic approaches for functional heartburn primarily involve esophageal pH monitoring and high-resolution manometry to assess acid exposure and motility disorders, distinguishing it from gastroesophageal reflux disease (GERD). Dyspepsia diagnosis often utilizes upper endoscopy to evaluate mucosal abnormalities and Helicobacter pylori testing to identify infectious causes. Both conditions require symptom assessment through validated questionnaires and exclusion of structural or inflammatory gastrointestinal diseases for accurate differentiation.
Overlapping Conditions and Misdiagnosis
Functional heartburn and dyspepsia often present with overlapping symptoms such as upper abdominal discomfort and burning sensations, leading to frequent misdiagnosis. Both conditions lack identifiable structural abnormalities in diagnostic tests, complicating differentiation and resulting in potential treatment delays. Accurate diagnosis requires comprehensive clinical evaluation and exclusion of gastroesophageal reflux disease (GERD) and peptic ulcer disease to prevent inappropriate therapies.
Treatment Options for Functional Heartburn
Treatment options for functional heartburn primarily include proton pump inhibitors (PPIs) to reduce acid production and improve symptoms, alongside lifestyle modifications such as dietary adjustments and weight management. When PPIs are ineffective, neuromodulators like tricyclic antidepressants or selective serotonin reuptake inhibitors may be prescribed to modulate pain perception. Behavioral therapies, including cognitive-behavioral therapy and relaxation techniques, can complement pharmacologic treatment by addressing stress-related symptom exacerbation.
Managing Dyspepsia Effectively
Managing dyspepsia effectively involves identifying underlying causes such as Helicobacter pylori infection, dietary triggers, and stress, which differ from the acid reflux-related symptoms seen in functional heartburn. Treatment strategies include prescribing proton pump inhibitors, recommending dietary modifications, and implementing lifestyle changes like stress reduction and weight management. Monitoring symptom patterns and response to therapy is crucial to distinguish dyspepsia from functional heartburn and ensure targeted interventions.
Lifestyle Modifications for Both Conditions
Functional heartburn and dyspepsia require distinct yet overlapping lifestyle modifications to manage symptoms effectively. For functional heartburn, reducing acidic food intake, avoiding late meals, and elevating the head during sleep can significantly decrease reflux episodes. Dyspepsia management emphasizes smaller, frequent meals, limiting fatty and spicy foods, and incorporating stress-reduction techniques to improve digestive comfort.
When to Seek Medical Advice
Seek medical advice for functional heartburn if frequent burning sensations persist despite over-the-counter antacids or lifestyle changes, especially when accompanied by difficulty swallowing, chest pain, or unintended weight loss. For dyspepsia, consult a healthcare provider if symptoms such as upper abdominal pain, bloating, or nausea continue for more than two weeks, worsen, or are associated with vomiting or black stools. Early evaluation is crucial to rule out serious conditions like gastroesophageal reflux disease, peptic ulcers, or gastric cancer.
Functional Heartburn Infographic
 libterm.com
libterm.com