Sclerosis refers to the abnormal hardening of body tissues, frequently affecting arteries, skin, or organs due to excessive fibrosis or calcification. This condition can lead to reduced elasticity and impaired function, commonly seen in diseases like multiple sclerosis or systemic sclerosis. Explore the rest of the article to understand the causes, symptoms, and treatment options that could impact your health.
Table of Comparison
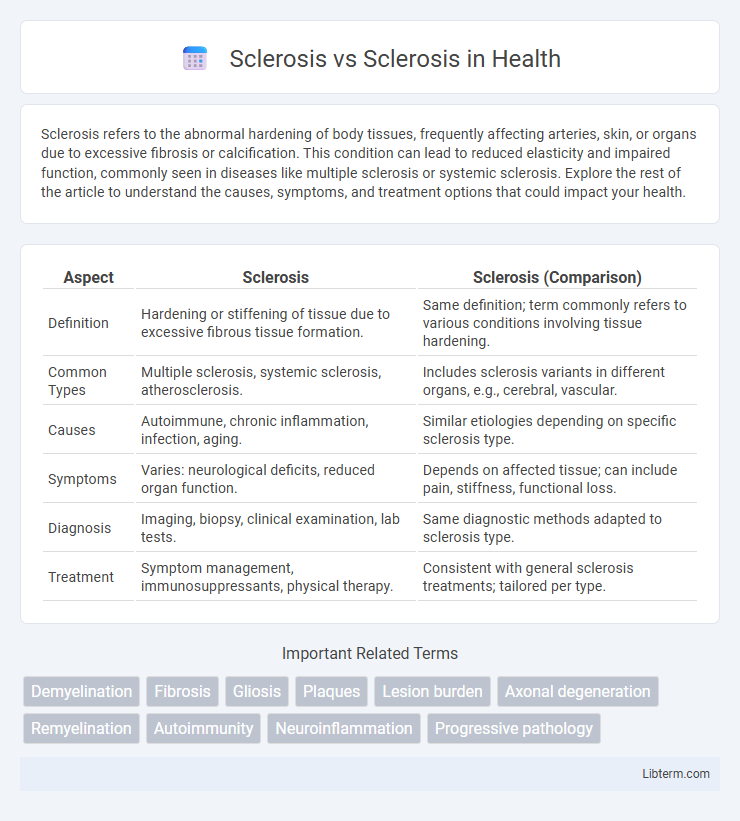
| Aspect | Sclerosis | Sclerosis (Comparison) |
|---|---|---|
| Definition | Hardening or stiffening of tissue due to excessive fibrous tissue formation. | Same definition; term commonly refers to various conditions involving tissue hardening. |
| Common Types | Multiple sclerosis, systemic sclerosis, atherosclerosis. | Includes sclerosis variants in different organs, e.g., cerebral, vascular. |
| Causes | Autoimmune, chronic inflammation, infection, aging. | Similar etiologies depending on specific sclerosis type. |
| Symptoms | Varies: neurological deficits, reduced organ function. | Depends on affected tissue; can include pain, stiffness, functional loss. |
| Diagnosis | Imaging, biopsy, clinical examination, lab tests. | Same diagnostic methods adapted to sclerosis type. |
| Treatment | Symptom management, immunosuppressants, physical therapy. | Consistent with general sclerosis treatments; tailored per type. |
Understanding the Term “Sclerosis”
Sclerosis refers to the abnormal hardening of body tissues due to excessive fibrosis or collagen buildup, often affecting arteries, nerves, or organs. Various types include multiple sclerosis, where immune-mediated nerve damage occurs, and atherosclerosis, characterized by plaque accumulation in arterial walls. Understanding sclerosis involves recognizing its role in chronic diseases marked by tissue stiffening and impaired function.
Common Types of Sclerosis
Multiple sclerosis (MS) primarily affects the central nervous system by damaging the myelin sheath, leading to symptoms such as muscle weakness and coordination issues. Systemic sclerosis, also known as scleroderma, is an autoimmune disorder characterized by skin thickening and organ fibrosis, often impacting the lungs, heart, and kidneys. Both conditions involve sclerosis, but MS targets nerve fibers, while systemic sclerosis involves connective tissue abnormalities.
Causes and Risk Factors of Different Scleroses
Multiple sclerosis results from an autoimmune attack on the central nervous system, with exact causes linked to genetic susceptibility and environmental triggers such as vitamin D deficiency and viral infections like Epstein-Barr virus. Amyotrophic lateral sclerosis primarily involves genetic mutations affecting motor neurons, with risk factors including age, family history, and exposure to environmental toxins like heavy metals. Other scleroses, like systemic sclerosis, arise from autoimmune dysfunction causing excessive collagen production, associated with risk factors such as female gender, certain infections, and occupational exposures to silica or organic solvents.
Multiple Sclerosis vs Systemic Sclerosis: Key Differences
Multiple Sclerosis (MS) is a chronic autoimmune disease targeting the central nervous system, characterized by demyelination and neurological impairment, whereas Systemic Sclerosis (SSc) primarily affects connective tissues, leading to skin thickening and fibrosis of internal organs. MS symptoms often include muscle weakness, coordination difficulties, and visual disturbances, while SSc manifests through Raynaud's phenomenon, skin hardening, and pulmonary fibrosis. Diagnostic differentiation relies on MRI findings for MS and autoantibody profiles such as anti-centromere or anti-Scl-70 for Systemic Sclerosis.
Symptoms Comparison: Neurological vs Connective Tissue Sclerosis
Neurological sclerosis, such as Multiple Sclerosis (MS), primarily presents with symptoms like muscle weakness, numbness, coordination difficulties, and vision problems caused by nerve damage in the central nervous system. In contrast, connective tissue sclerosis, including Systemic Sclerosis (Scleroderma), manifests with skin thickening, Raynaud's phenomenon, joint stiffness, and internal organ fibrosis due to abnormal collagen deposition. Differentiating these conditions relies on identifying neurological impairments versus connective tissue abnormalities through clinical evaluation and imaging studies.
Diagnostic Methods for Various Sclerotic Diseases
Diagnostic methods for various sclerotic diseases primarily include advanced imaging techniques such as MRI and CT scans, which provide detailed visualization of tissue hardening and lesion distribution. Blood tests and biopsy samples offer crucial molecular and histopathological data, facilitating differentiation between multiple sclerosis, systemic sclerosis, and other sclerotic conditions. Electrophysiological studies and serological markers further enhance diagnostic accuracy by revealing nerve conduction abnormalities and specific autoantibodies associated with sclerotic disorders.
Treatment Approaches: Medication and Therapy
Treatment approaches for multiple sclerosis often involve disease-modifying therapies such as interferons, glatiramer acetate, and newer oral medications like fingolimod to reduce relapse rates and slow progression. In contrast, systemic sclerosis management primarily includes immunosuppressive agents like methotrexate or cyclophosphamide to control inflammation and fibrosis, alongside physical therapy to maintain skin and joint flexibility. Both conditions may benefit from symptomatic treatments, but their medication regimens target fundamentally different pathological mechanisms specific to neurological or connective tissue involvement.
Prognosis and Life Expectancy
Sclerosis varies significantly between types, such as multiple sclerosis (MS) and systemic sclerosis, with differing prognoses and life expectancy impacts. Multiple sclerosis often involves a variable course with many patients maintaining a near-normal life expectancy, whereas systemic sclerosis, especially with organ involvement, can lead to a reduced lifespan due to complications like pulmonary hypertension or renal failure. Early diagnosis and advances in treatment improve outcomes, but prognosis largely depends on disease progression and organ damage severity.
Coping Strategies and Lifestyle Adaptations
Coping strategies for Multiple Sclerosis (MS) primarily include stress management techniques, physical therapy, and cognitive behavioral therapy to address fatigue and cognitive challenges. In contrast, coping with Systemic Sclerosis (SSc) emphasizes skin care routines, managing organ complications, and tailored exercise plans to maintain mobility. Both conditions benefit from a balanced diet, regular medical follow-ups, and emotional support to enhance quality of life and disease management.
Recent Research and Future Directions in Sclerotic Diseases
Recent research in sclerotic diseases, including multiple sclerosis (MS) and systemic sclerosis (SSc), emphasizes molecular pathways such as fibrosis and immune dysregulation for targeted therapies. Advances in biomarkers, like neurofilament light chain in MS and autoantibodies in SSc, enhance early diagnosis and personalized treatment strategies. Future directions focus on gene editing and regenerative medicine approaches to reverse tissue damage and improve long-term patient outcomes.
Sclerosis Infographic
 libterm.com
libterm.com