Hypernatremia occurs when sodium levels in your blood become dangerously high, often due to dehydration or impaired kidney function. This imbalance can lead to symptoms such as confusion, muscle twitching, and seizures if not addressed promptly. Discover effective strategies to recognize, treat, and prevent hypernatremia by reading the full article.
Table of Comparison
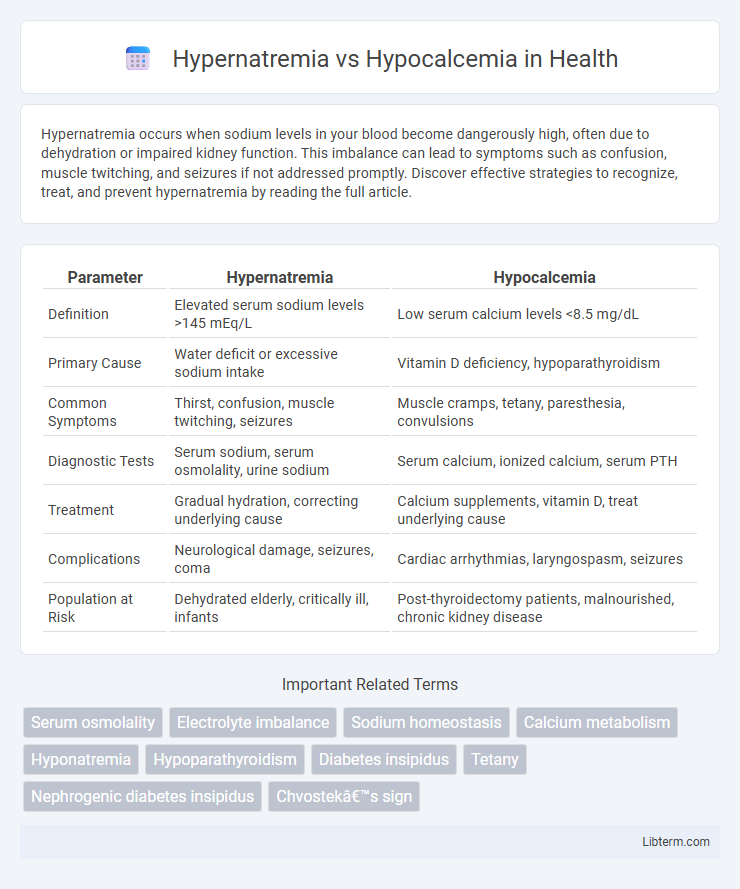
| Parameter | Hypernatremia | Hypocalcemia |
|---|---|---|
| Definition | Elevated serum sodium levels >145 mEq/L | Low serum calcium levels <8.5 mg/dL |
| Primary Cause | Water deficit or excessive sodium intake | Vitamin D deficiency, hypoparathyroidism |
| Common Symptoms | Thirst, confusion, muscle twitching, seizures | Muscle cramps, tetany, paresthesia, convulsions |
| Diagnostic Tests | Serum sodium, serum osmolality, urine sodium | Serum calcium, ionized calcium, serum PTH |
| Treatment | Gradual hydration, correcting underlying cause | Calcium supplements, vitamin D, treat underlying cause |
| Complications | Neurological damage, seizures, coma | Cardiac arrhythmias, laryngospasm, seizures |
| Population at Risk | Dehydrated elderly, critically ill, infants | Post-thyroidectomy patients, malnourished, chronic kidney disease |
Introduction to Hypernatremia and Hypocalcemia
Hypernatremia is characterized by elevated sodium levels exceeding 145 mEq/L, often resulting from dehydration, impaired kidney function, or excessive salt intake, leading to neurological symptoms such as confusion, seizures, and muscle twitching. Hypocalcemia involves calcium levels below 8.5 mg/dL, frequently caused by hypoparathyroidism, vitamin D deficiency, or chronic kidney disease, manifesting as muscle cramps, tetany, and cardiac arrhythmias. Both electrolyte imbalances require prompt diagnosis and management due to their significant impact on cellular function and systemic homeostasis.
Key Differences Between Hypernatremia and Hypocalcemia
Hypernatremia is characterized by an elevated sodium level in the blood, typically above 145 mEq/L, whereas hypocalcemia refers to abnormally low calcium levels, generally below 8.5 mg/dL. Key differences include their primary regulatory systems: sodium balance is mainly controlled by renal function and aldosterone, while calcium homeostasis depends on parathyroid hormone, vitamin D, and calcitonin levels. Clinical manifestations of hypernatremia often involve neurological symptoms like confusion and seizures due to cellular dehydration, whereas hypocalcemia commonly presents with neuromuscular irritability such as tetany and muscle spasms.
Causes of Hypernatremia
Hypernatremia primarily results from water loss exceeding sodium loss due to dehydration, diabetes insipidus, or excessive salt intake. Other causes include impaired thirst mechanism, gastrointestinal losses such as vomiting and diarrhea, and renal dysfunction leading to inefficient water reabsorption. In contrast, hypocalcemia is mainly caused by hypoparathyroidism, vitamin D deficiency, and chronic kidney disease, which disrupt calcium metabolism.
Causes of Hypocalcemia
Hypocalcemia primarily results from vitamin D deficiency, impaired parathyroid hormone secretion, or chronic kidney disease disrupting calcium metabolism. Other causes include magnesium deficiency, acute pancreatitis, and certain medications such as bisphosphonates or anticonvulsants. Unlike hypernatremia, which stems from sodium imbalance, hypocalcemia directly impacts neuromuscular function due to low serum calcium levels.
Clinical Manifestations of Hypernatremia
Hypernatremia presents clinically with symptoms such as intense thirst, dry mucous membranes, and neurological disturbances including confusion, lethargy, and seizures due to cellular dehydration in the brain. In contrast, hypocalcemia primarily manifests with neuromuscular irritability, including tetany, muscle cramps, and positive Chvostek and Trousseau signs. Understanding these distinct clinical manifestations aids in differential diagnosis and targeted management of electrolyte imbalances.
Clinical Manifestations of Hypocalcemia
Hypocalcemia manifests clinically with neuromuscular irritability, including symptoms such as tetany, muscle cramps, and paresthesia around the mouth or in the extremities. Chvostek's and Trousseau's signs are key indicators, demonstrating facial muscle twitching and carpopedal spasm, respectively. Severe hypocalcemia can lead to seizures, prolonged QT interval on ECG, and cardiac arrhythmias.
Diagnostic Approaches in Electrolyte Imbalances
Diagnostic approaches for hypernatremia primarily involve serum sodium measurement above 145 mEq/L, assessment of plasma osmolality, and evaluation of patient hydration status to distinguish between causes such as water loss or sodium gain. Hypocalcemia diagnosis requires total and ionized serum calcium level testing below 8.5 mg/dL, measurement of parathyroid hormone (PTH), vitamin D levels, and phosphate concentrations to identify underlying etiologies like hypoparathyroidism or vitamin D deficiency. Both conditions benefit from comprehensive electrolyte panels and clinical correlation to guide appropriate treatment strategies.
Treatment Strategies for Hypernatremia
Hypernatremia treatment focuses on gradual normalization of serum sodium levels to prevent cerebral edema, primarily through controlled administration of hypotonic fluids or oral water intake in mild cases. Intravenous isotonic or hypotonic saline may be used depending on volume status, while identifying and correcting the underlying cause such as diabetes insipidus or inadequate water intake is crucial. Monitoring serum sodium levels every 2 to 4 hours ensures safe correction rates, typically not exceeding 10-12 mEq/L per day to avoid osmotic demyelination syndrome.
Management of Hypocalcemia
Management of hypocalcemia involves rapid calcium supplementation, typically with intravenous calcium gluconate for severe cases and oral calcium salts for mild to moderate deficiencies. Monitoring serum calcium levels, along with magnesium and vitamin D status, is crucial to address underlying causes and prevent recurrence. Correcting hypocalcemia effectively reduces neuromuscular irritability and cardiac complications associated with the condition.
Prevention and Prognosis of Electrolyte Disorders
Hypernatremia prevention involves maintaining adequate hydration and monitoring sodium intake, especially in vulnerable populations like the elderly and critically ill. Hypocalcemia prevention focuses on ensuring sufficient dietary calcium and vitamin D levels while managing underlying conditions such as hypoparathyroidism or chronic kidney disease. Prognosis for both electrolyte disorders improves significantly with early detection and targeted treatment, reducing complications like neurological impairment in hypernatremia and cardiac arrhythmias in hypocalcemia.
Hypernatremia Infographic
 libterm.com
libterm.com