Coagulation is a critical process within hemostasis that stops bleeding by forming blood clots at injury sites. This complex cascade involves platelets, clotting factors, and fibrin to stabilize the wound and prevent excessive blood loss. Discover how understanding this vital mechanism can empower your knowledge of bleeding disorders and treatments in the full article.
Table of Comparison
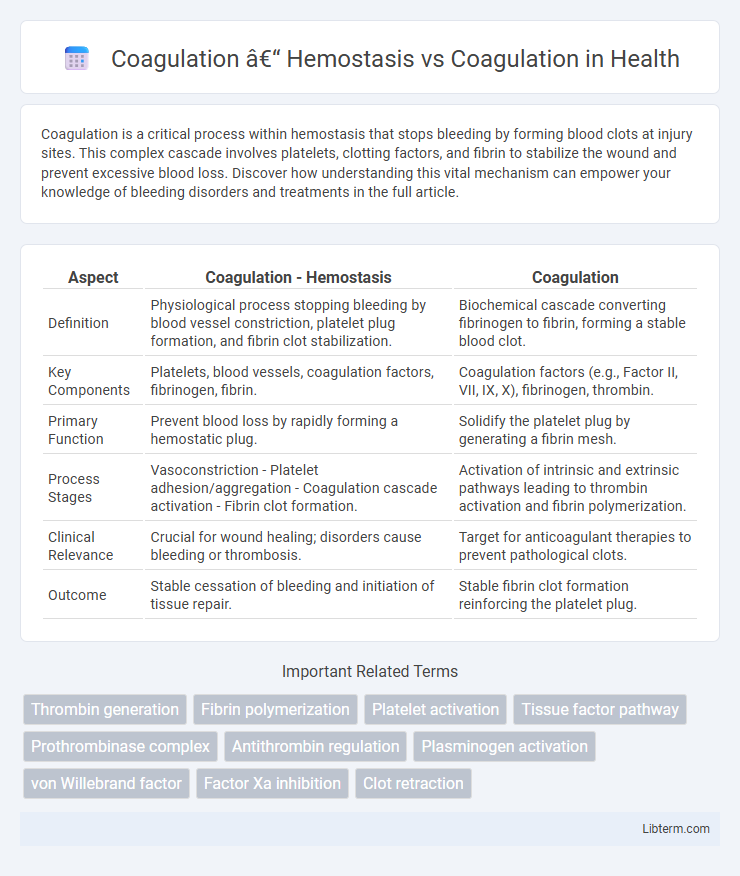
| Aspect | Coagulation - Hemostasis | Coagulation |
|---|---|---|
| Definition | Physiological process stopping bleeding by blood vessel constriction, platelet plug formation, and fibrin clot stabilization. | Biochemical cascade converting fibrinogen to fibrin, forming a stable blood clot. |
| Key Components | Platelets, blood vessels, coagulation factors, fibrinogen, fibrin. | Coagulation factors (e.g., Factor II, VII, IX, X), fibrinogen, thrombin. |
| Primary Function | Prevent blood loss by rapidly forming a hemostatic plug. | Solidify the platelet plug by generating a fibrin mesh. |
| Process Stages | Vasoconstriction - Platelet adhesion/aggregation - Coagulation cascade activation - Fibrin clot formation. | Activation of intrinsic and extrinsic pathways leading to thrombin activation and fibrin polymerization. |
| Clinical Relevance | Crucial for wound healing; disorders cause bleeding or thrombosis. | Target for anticoagulant therapies to prevent pathological clots. |
| Outcome | Stable cessation of bleeding and initiation of tissue repair. | Stable fibrin clot formation reinforcing the platelet plug. |
Introduction to Coagulation and Hemostasis
Coagulation and hemostasis are critical physiological processes that prevent excessive bleeding following vascular injury by forming a stable blood clot. Hemostasis encompasses vascular constriction, platelet activation, and the coagulation cascade, which involves a complex series of enzymatic reactions converting fibrinogen into fibrin to stabilize the platelet plug. Efficient coagulation ensures blood fluidity under normal conditions while rapidly initiating clot formation to maintain vascular integrity during tissue damage.
Defining Hemostasis
Hemostasis is the physiological process that stops bleeding at the site of blood vessel injury by forming a stable blood clot, involving vascular constriction, platelet activation, and coagulation pathways. Coagulation is a critical component of hemostasis, specifically referring to the cascade of enzymatic reactions that lead to fibrin mesh formation, stabilizing the platelet plug. Understanding hemostasis encompasses both vascular and cellular responses along with coagulation factors to maintain blood fluidity and prevent hemorrhage.
Understanding Coagulation
Understanding coagulation involves recognizing the complex physiological process where blood transforms from a liquid to a gel, forming clots to prevent excessive bleeding. Hemostasis encompasses coagulation as one of its critical phases, alongside vascular spasm and platelet aggregation, working collectively to maintain vascular integrity. The coagulation cascade activates clotting factors in a precise sequence, leading to fibrin mesh formation that stabilizes the platelet plug during hemostasis.
Key Steps in Hemostasis
Hemostasis involves a series of key steps including vascular spasm, platelet plug formation, and coagulation, which work together to prevent bleeding. Platelet activation and aggregation form the initial plug, while the coagulation cascade stabilizes this plug through fibrin mesh formation. The coagulation process itself consists of intrinsic, extrinsic, and common pathways that activate clotting factors, culminating in the generation of thrombin and the conversion of fibrinogen to fibrin.
The Coagulation Cascade: Overview
The coagulation cascade is a complex series of enzymatic reactions essential for hemostasis, involving intrinsic, extrinsic, and common pathways that lead to fibrin clot formation. Key factors such as Factor VIII, Factor IX, and Factor X activate sequentially, converting prothrombin to thrombin, which then polymerizes fibrinogen into a stable fibrin mesh. Disruptions in the coagulation cascade can result in bleeding disorders or thrombosis, highlighting its critical role in maintaining vascular integrity after injury.
Hemostasis vs Coagulation: Core Differences
Hemostasis is the physiological process that stops bleeding by forming a stable blood clot, involving vascular constriction, platelet activation, and coagulation cascade activation. Coagulation specifically refers to the enzymatic cascade that leads to fibrin mesh formation, stabilizing the platelet plug during hemostasis. The core difference lies in hemostasis being an overarching process encompassing multiple steps, while coagulation is a critical subset focused on blood clot formation.
Platelets in Hemostasis and Coagulation
Platelets play a crucial role in hemostasis by rapidly adhering to damaged blood vessel walls, forming a temporary plug to prevent blood loss. In coagulation, platelets provide a surface for the assembly of clotting factors that produce fibrin, stabilizing the initial platelet plug. This dual function of platelets integrates vascular repair and blood clot formation, essential for effective hemostatic response.
Disorders Affecting Hemostasis and Coagulation
Disorders affecting hemostasis and coagulation include conditions like hemophilia, characterized by a deficiency in clotting factors leading to impaired clot formation, and thrombocytopenia, where low platelet counts disrupt primary hemostasis. Other significant disorders such as disseminated intravascular coagulation (DIC) involve pathological activation of coagulation pathways resulting in widespread clotting and bleeding. Accurate diagnosis and management rely on understanding the distinct roles of platelet function, clotting factor activity, and fibrinolysis within the hemostatic process.
Clinical Significance of Hemostasis and Coagulation
Hemostasis is a critical physiological process that prevents excessive bleeding by forming a stable blood clot through vessel constriction, platelet aggregation, and coagulation cascade activation. Coagulation specifically refers to the enzymatic cascade converting fibrinogen to fibrin, stabilizing the platelet plug and ensuring wound closure. Clinically, impaired hemostasis or coagulation disorders can lead to hemorrhagic conditions, thrombosis, or bleeding complications during surgery, necessitating precise diagnostic and therapeutic interventions.
Conclusion: Integrating Hemostasis and Coagulation
Hemostasis is the physiological process that stops bleeding through vascular constriction, platelet aggregation, and clot formation, while coagulation is the biochemical cascade that reinforces the platelet plug by generating fibrin. Integrating hemostasis and coagulation is essential for maintaining vascular integrity and preventing excessive bleeding or thrombosis. Effective clinical management requires understanding their interplay to optimize treatments for bleeding disorders and thrombotic conditions.
Coagulation – Hemostasis Infographic
 libterm.com
libterm.com