Hyperkalemia is a condition characterized by elevated potassium levels in the bloodstream, which can disrupt normal heart and muscle function. Identifying symptoms early and managing dietary potassium intake are crucial to prevent serious complications like cardiac arrhythmias. Explore this article to understand the causes, symptoms, and effective treatment options for your health.
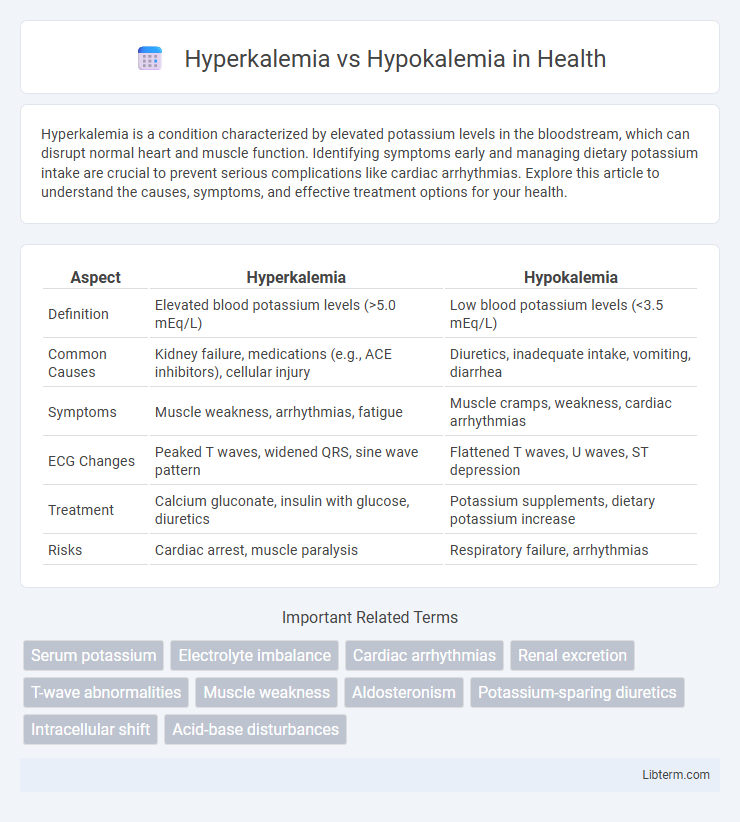
Table of Comparison
| Aspect | Hyperkalemia | Hypokalemia |
|---|---|---|
| Definition | Elevated blood potassium levels (>5.0 mEq/L) | Low blood potassium levels (<3.5 mEq/L) |
| Common Causes | Kidney failure, medications (e.g., ACE inhibitors), cellular injury | Diuretics, inadequate intake, vomiting, diarrhea |
| Symptoms | Muscle weakness, arrhythmias, fatigue | Muscle cramps, weakness, cardiac arrhythmias |
| ECG Changes | Peaked T waves, widened QRS, sine wave pattern | Flattened T waves, U waves, ST depression |
| Treatment | Calcium gluconate, insulin with glucose, diuretics | Potassium supplements, dietary potassium increase |
| Risks | Cardiac arrest, muscle paralysis | Respiratory failure, arrhythmias |
Introduction to Potassium Imbalances
Potassium imbalances, specifically hyperkalemia and hypokalemia, impact cellular function and cardiac health by disrupting the normal potassium ion gradient essential for nerve impulse transmission and muscle contraction. Hyperkalemia involves elevated serum potassium levels above 5.0 mmol/L, increasing the risk of life-threatening cardiac arrhythmias, while hypokalemia denotes serum potassium below 3.5 mmol/L, often causing muscle weakness and cardiac conduction abnormalities. Both conditions require precise potassium regulation to maintain electrolyte balance, renal function, and overall cardiovascular stability.
What is Hyperkalemia?
Hyperkalemia is a medical condition characterized by elevated potassium levels in the blood, typically above 5.0 mEq/L, disrupting normal cellular function and potentially leading to cardiac arrhythmias. It commonly results from impaired kidney function, excessive potassium intake, or certain medications like potassium-sparing diuretics. Monitoring serum potassium and addressing underlying causes are critical to preventing complications associated with hyperkalemia.
What is Hypokalemia?
Hypokalemia is a medical condition characterized by abnormally low levels of potassium in the bloodstream, typically defined as a serum potassium concentration below 3.5 mmol/L. This electrolyte imbalance can cause symptoms such as muscle weakness, cramps, fatigue, and in severe cases, cardiac arrhythmias due to impaired electrical conduction in the heart. Common causes include excessive potassium loss from conditions like vomiting, diarrhea, diuretic use, or inadequate potassium intake.
Causes of Hyperkalemia
Hyperkalemia is primarily caused by impaired renal potassium excretion due to conditions such as chronic kidney disease, acute kidney injury, or the use of potassium-sparing diuretics and certain medications like ACE inhibitors and ARBs. Excessive potassium intake or cellular release from tissue breakdown in rhabdomyolysis, hemolysis, or metabolic acidosis also contributes to hyperkalemia. In contrast, hypokalemia results from excessive potassium loss via vomiting, diarrhea, or diuretics, and inadequate dietary potassium intake.
Causes of Hypokalemia
Hypokalemia is primarily caused by excessive potassium loss due to factors such as prolonged vomiting, diarrhea, diuretic use, and certain kidney disorders. Inadequate dietary potassium intake and conditions leading to intracellular potassium shifts, like insulin administration or alkalosis, also contribute to low serum potassium levels. Understanding these causes is crucial for diagnosing and treating hypokalemia effectively, as it contrasts with hyperkalemia, where elevated potassium results from impaired renal excretion or cell lysis.
Symptoms: Hyperkalemia vs Hypokalemia
Hyperkalemia symptoms include muscle weakness, fatigue, palpitations, and in severe cases, cardiac arrhythmias or paralysis due to elevated potassium levels disrupting normal cellular function. Hypokalemia manifests with muscle cramps, weakness, constipation, and arrhythmias caused by decreased potassium affecting nerve and muscle excitability. Both conditions require careful monitoring of serum potassium levels to prevent life-threatening complications.
Diagnostic Approaches and Lab Findings
Hyperkalemia diagnostic approaches include serum potassium measurement, ECG changes such as peaked T waves, and assessing renal function to identify causes like acute kidney injury. Hypokalemia diagnosis involves serum potassium testing, ECG signs like flattened T waves or U waves, and evaluation of causes such as diuretic use or gastrointestinal losses. Laboratory findings for hyperkalemia show elevated potassium levels above 5.0 mmol/L, whereas hypokalemia is characterized by potassium levels below 3.5 mmol/L, with acid-base status and renal potassium excretion tests aiding differential diagnosis.
Treatment Strategies for Hyperkalemia
Treatment strategies for hyperkalemia prioritize stabilizing cardiac membranes with intravenous calcium gluconate, followed by shifting potassium intracellularly using insulin with glucose or beta-2 agonists like albuterol. Enhanced potassium elimination is achieved through diuretics, sodium polystyrene sulfonate, or dialysis in severe cases. Continuous monitoring of serum potassium levels and ECG changes is crucial to prevent life-threatening arrhythmias.
Treatment Strategies for Hypokalemia
Treatment strategies for hypokalemia primarily involve potassium supplementation through oral or intravenous administration to restore normal serum potassium levels. Addressing underlying causes such as diuretic use, gastrointestinal losses, or magnesium deficiency is essential to prevent recurrence. Monitoring cardiac function and serum electrolytes during treatment helps avoid complications like arrhythmias and ensures effective potassium repletion.
Prevention and Long-term Management
Maintaining balanced potassium levels through dietary regulation, including potassium-rich foods for hypokalemia and potassium-limited intake for hyperkalemia, is crucial for prevention and long-term management. Regular monitoring of serum potassium, especially in patients with kidney disease or on medications like diuretics and ACE inhibitors, helps detect imbalances early and tailor treatment. Chronic management may involve the use of potassium supplements in hypokalemia or potassium binders and dialysis in severe hyperkalemia cases to prevent cardiac and neuromuscular complications.
Hyperkalemia Infographic
 libterm.com
libterm.com