Pleural effusion occurs when excess fluid builds up between the layers of the pleura surrounding the lungs, causing difficulty in breathing and chest pain. Common causes include infections, heart failure, and malignancies, which require timely diagnosis and appropriate treatment to prevent complications. Explore the article to understand symptoms, causes, and effective management strategies for your health.
Table of Comparison
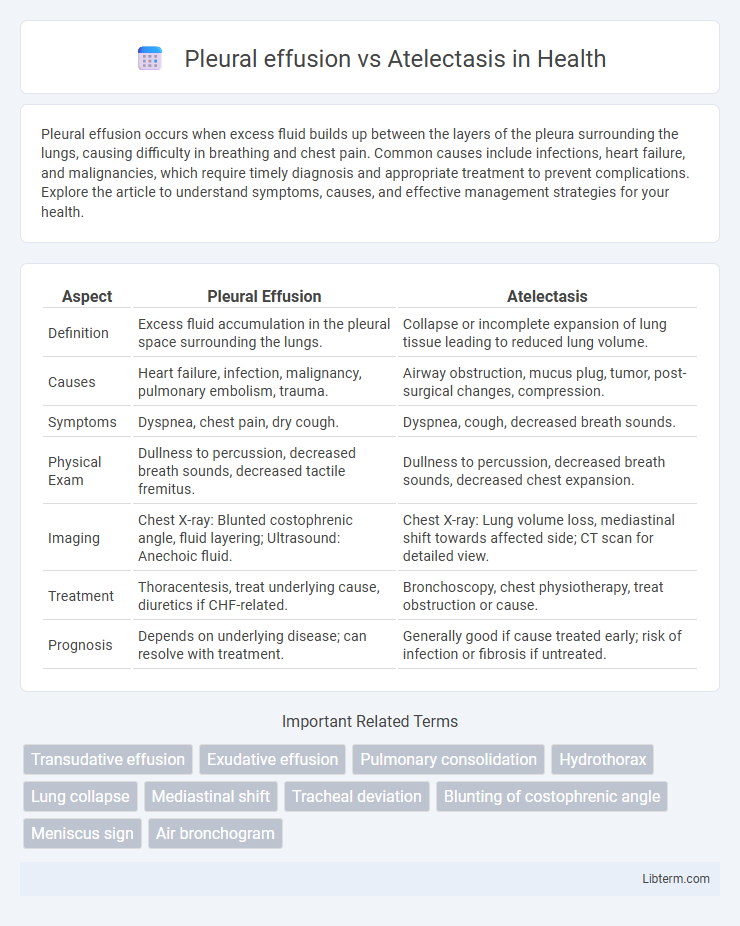
| Aspect | Pleural Effusion | Atelectasis |
|---|---|---|
| Definition | Excess fluid accumulation in the pleural space surrounding the lungs. | Collapse or incomplete expansion of lung tissue leading to reduced lung volume. |
| Causes | Heart failure, infection, malignancy, pulmonary embolism, trauma. | Airway obstruction, mucus plug, tumor, post-surgical changes, compression. |
| Symptoms | Dyspnea, chest pain, dry cough. | Dyspnea, cough, decreased breath sounds. |
| Physical Exam | Dullness to percussion, decreased breath sounds, decreased tactile fremitus. | Dullness to percussion, decreased breath sounds, decreased chest expansion. |
| Imaging | Chest X-ray: Blunted costophrenic angle, fluid layering; Ultrasound: Anechoic fluid. | Chest X-ray: Lung volume loss, mediastinal shift towards affected side; CT scan for detailed view. |
| Treatment | Thoracentesis, treat underlying cause, diuretics if CHF-related. | Bronchoscopy, chest physiotherapy, treat obstruction or cause. |
| Prognosis | Depends on underlying disease; can resolve with treatment. | Generally good if cause treated early; risk of infection or fibrosis if untreated. |
Understanding Pleural Effusion and Atelectasis
Pleural effusion is the accumulation of excess fluid in the pleural space, often caused by infections, heart failure, or malignancies, leading to impaired lung expansion and respiratory distress. Atelectasis refers to the partial or complete collapse of lung tissue due to airway obstruction, compression, or surfactant deficiency, resulting in reduced gas exchange and hypoxia. Differentiating pleural effusion from atelectasis is essential in imaging studies, where effusion appears as fluid opacity with meniscus sign on chest X-rays, while atelectasis shows volume loss with mediastinal shift toward the affected side.
Definition and Pathophysiology
Pleural effusion is the accumulation of excess fluid in the pleural space, often caused by inflammation, infection, or malignancy, leading to impaired lung expansion. Atelectasis refers to the collapse or incomplete expansion of lung tissue, resulting from airway obstruction, compression, or surfactant deficiency, which reduces alveolar ventilation. Both conditions disrupt normal respiratory function but differ in underlying mechanisms: fluid buildup in pleural effusion versus lung tissue collapse in atelectasis.
Causes and Risk Factors
Pleural effusion occurs due to excess fluid accumulation in the pleural space, commonly caused by conditions such as congestive heart failure, pneumonia, malignancies, and pulmonary embolism. Atelectasis results from lung tissue collapse, often triggered by airway obstruction, postoperative complications, or underlying chronic lung diseases like cystic fibrosis or chronic obstructive pulmonary disease (COPD). Risk factors for pleural effusion include heart or kidney failure and infections, while atelectasis risk increases with immobility, smoking, and prolonged anesthesia exposure.
Clinical Presentation and Symptoms
Pleural effusion typically presents with dyspnea, pleuritic chest pain, and decreased breath sounds on the affected side, often accompanied by dullness to percussion and reduced tactile fremitus. Atelectasis manifests with similar symptoms, including dyspnea and decreased breath sounds, but is often associated with mediastinal shift toward the affected lung and absence of pleural fluid on imaging. Both conditions can cause hypoxemia, but clinical examination and chest imaging help differentiate pleural effusion's pleural fluid accumulation from atelectasis's alveolar collapse.
Diagnostic Techniques and Imaging Findings
Pleural effusion typically appears on chest X-rays as a homogenous opacity with a meniscus sign and blunting of the costophrenic angle, while ultrasound reveals an anechoic or hypoechoic fluid collection useful for guided thoracentesis. Atelectasis shows volume loss on imaging characterized by increased lung opacity, displacement of fissures, and elevation of the diaphragm on the affected side, with CT scans providing detailed visualization of bronchial obstruction or compression. Diagnostic techniques for pleural effusion involve thoracentesis to analyze pleural fluid, whereas atelectasis diagnosis relies on imaging combined with clinical evaluation to identify the underlying cause such as mucus plugging or external compression.
Differences in Physical Examination
Pleural effusion typically presents with decreased or absent breath sounds, dullness to percussion, and diminished tactile fremitus over the affected area due to fluid accumulation in the pleural space. Atelectasis often reveals decreased breath sounds and dullness to percussion as well but is distinguished by increased tactile fremitus caused by lung tissue collapse and volume loss. Tracheal deviation toward the affected side occurs in atelectasis, whereas pleural effusion may cause deviation away from the fluid collection.
Complications and Associated Conditions
Pleural effusion often leads to complications such as respiratory distress, infection (empyema), and fibrothorax, frequently associated with conditions like congestive heart failure, pneumonia, and malignancies. Atelectasis can cause hypoxemia, superimposed infections, and respiratory failure, commonly linked to obstructive lung diseases, post-surgical immobility, and pleural effusion itself. Both conditions may coexist, exacerbating pulmonary compromise and complicating clinical management.
Treatment Approaches
Treatment approaches for pleural effusion primarily involve thoracentesis to drain excess fluid and addressing the underlying cause, such as infections or malignancies, often supplemented by antibiotics or chemotherapy. Atelectasis management centers on improving lung expansion through techniques like incentive spirometry, chest physiotherapy, and positive airway pressure therapy, while severe cases may require bronchoscopy to remove airway obstructions. Both conditions necessitate targeted therapies that reduce symptoms and prevent respiratory complications, with pleural effusion often demanding more invasive interventions compared to atelectasis.
Prognosis and Patient Outcomes
Pleural effusion prognosis depends on the underlying cause, with malignant or infectious effusions associated with higher morbidity and mortality, while simple effusions often resolve with treatment. Atelectasis prognosis varies based on etiology, with reversible causes like mucus plugging generally showing good patient outcomes, whereas sustained or extensive atelectasis can lead to respiratory complications and prolonged hospitalization. Early diagnosis and targeted management in both conditions significantly improve patient outcomes by reducing respiratory distress and preventing long-term pulmonary impairment.
Key Differences: Pleural Effusion vs Atelectasis
Pleural effusion involves the accumulation of excess fluid in the pleural space, causing lung compression and impaired respiratory function, while atelectasis refers to the collapse or incomplete expansion of lung tissue leading to reduced gas exchange. Pleural effusion is identified through imaging tests showing fluid layers, often with symptoms like chest pain and dyspnea, whereas atelectasis is characterized by lung volume loss and may result from airway obstruction or hypoventilation. Treatment for pleural effusion targets fluid removal or underlying causes, whereas atelectasis management focuses on clearing airway obstructions and re-expanding the affected lung tissue.
Pleural effusion Infographic
 libterm.com
libterm.com