Transudate is a fluid that accumulates in body cavities due to imbalances in hydrostatic or oncotic pressure, typically clear and low in protein content. It often indicates systemic conditions such as heart failure, liver cirrhosis, or nephrotic syndrome rather than local inflammation. Explore the rest of the article to understand the causes, characteristics, and clinical significance of transudates in detail.
Table of Comparison
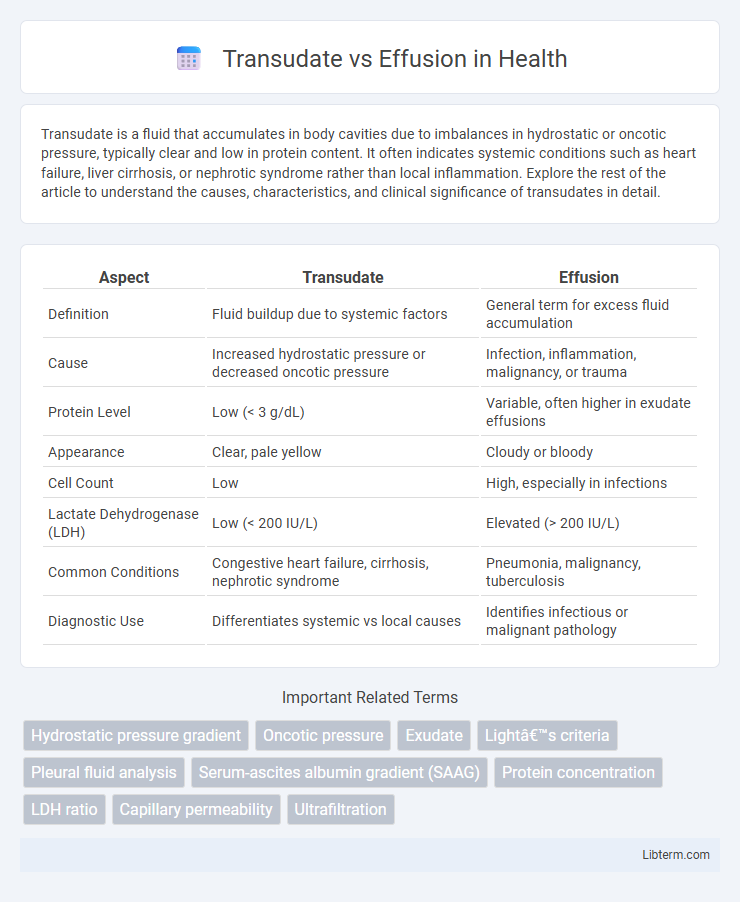
| Aspect | Transudate | Effusion |
|---|---|---|
| Definition | Fluid buildup due to systemic factors | General term for excess fluid accumulation |
| Cause | Increased hydrostatic pressure or decreased oncotic pressure | Infection, inflammation, malignancy, or trauma |
| Protein Level | Low (< 3 g/dL) | Variable, often higher in exudate effusions |
| Appearance | Clear, pale yellow | Cloudy or bloody |
| Cell Count | Low | High, especially in infections |
| Lactate Dehydrogenase (LDH) | Low (< 200 IU/L) | Elevated (> 200 IU/L) |
| Common Conditions | Congestive heart failure, cirrhosis, nephrotic syndrome | Pneumonia, malignancy, tuberculosis |
| Diagnostic Use | Differentiates systemic vs local causes | Identifies infectious or malignant pathology |
Introduction to Transudate and Effusion
Transudate and effusion represent distinct fluid accumulations within body cavities, with transudate characterized by low protein content and clear appearance due to systemic factors like heart failure or hypoalbuminemia. Effusion, often used interchangeably with exudate, involves fluid rich in proteins and cellular elements, typically resulting from inflammation, infection, or malignancy. Understanding the biochemical and cellular differences between transudate and effusion is crucial for accurate diagnosis and targeted clinical management.
Defining Transudate: Key Characteristics
Transudate is a type of fluid characterized by low protein content, typically less than 3 g/dL, and low lactate dehydrogenase (LDH) levels, distinguishing it from exudate. It results from systemic factors that alter hydrostatic or oncotic pressure, such as congestive heart failure or cirrhosis, leading to fluid accumulation without inflammation or increased vascular permeability. The specific gravity of transudate usually remains below 1.015, aiding in differentiation from effusion caused by inflammatory or infectious processes.
Understanding Effusion: An Overview
Effusion refers to the abnormal accumulation of fluid in body cavities such as the pleural, peritoneal, or pericardial spaces, distinguishing it from transudate by its higher protein content and cellularity. Recognizing the biochemical and cytological characteristics of effusion aids in diagnosing underlying conditions like infections, malignancies, or inflammatory diseases. Accurate analysis of effusion, including lactate dehydrogenase (LDH) levels and specific gravity, is essential for effective clinical management and treatment planning.
Causes of Transudative Fluid Accumulation
Transudative fluid accumulation primarily results from systemic conditions that alter hydrostatic or oncotic pressure, such as congestive heart failure, liver cirrhosis, and nephrotic syndrome. These disturbances lead to the movement of low-protein fluid across membranes without significant inflammation or increased vascular permeability. Understanding these causes is essential for distinguishing transudates from exudative pleural effusions, which are typically caused by infections, malignancies, or inflammatory diseases.
Common Etiologies of Effusion
Effusions commonly arise from conditions such as congestive heart failure, pneumonia, malignancies, and pulmonary embolism, which cause increased vascular permeability or impaired lymphatic drainage. Inflammatory diseases like tuberculosis and autoimmune disorders also frequently lead to effusion by inducing pleural inflammation and fluid accumulation. Recognizing these etiologies is critical for accurate diagnosis and appropriate management of pleural effusions.
Diagnostic Criteria: Differentiating Transudate from Effusion
Differentiating transudate from exudate effusion primarily relies on Light's criteria, which evaluate pleural fluid protein and lactate dehydrogenase (LDH) levels compared to serum values; transudates typically show pleural fluid protein/serum protein ratio less than 0.5, pleural fluid LDH/serum LDH ratio less than 0.6, and pleural fluid LDH less than two-thirds the upper limit of normal serum LDH. Measuring pleural fluid cholesterol and albumin gradients further assists diagnosis, with effusions demonstrating higher cholesterol levels and lower albumin gradients than transudates. Identifying these biochemical markers allows clinicians to distinguish between systemic causes like congestive heart failure in transudates and local inflammatory or malignant processes in exudates.
Laboratory Analysis: Key Parameters
Laboratory analysis distinguishes transudate from effusion primarily by assessing the protein concentration, lactate dehydrogenase (LDH) levels, and specific gravity in pleural fluid. Transudates typically present with low protein (<3 g/dL), low LDH (<200 IU/L), and specific gravity less than 1.015, reflecting systemic factors like heart failure or cirrhosis. In contrast, exudative effusions exhibit elevated protein (>3 g/dL), high LDH (>200 IU/L), and specific gravity above 1.020, indicative of inflammation or malignancy in conditions such as pneumonia or cancer.
Clinical Manifestations and Symptoms
Transudates typically present with clear, pale fluid accumulation often associated with systemic conditions like heart failure, liver cirrhosis, or nephrotic syndrome, resulting in symptoms such as dyspnea and peripheral edema without significant inflammation. Effusions, particularly exudates, commonly indicate localized inflammation or infection, displaying cloudy or purulent fluid and symptoms including fever, chest pain, and pleuritic discomfort. Differentiating these entities relies on clinical presentation and diagnostic analysis, such as fluid protein concentration and lactate dehydrogenase levels, to guide appropriate management.
Importance in Disease Diagnosis and Management
Transudate and effusion differentiation is crucial in disease diagnosis and management because transudates typically indicate systemic conditions like heart failure or cirrhosis, whereas exudates suggest localized inflammation or infection such as pneumonia or malignancy. Accurate analysis of pleural fluid characteristics, including protein concentration and lactate dehydrogenase levels, guides targeted therapeutic interventions and prognosis assessment. Timely distinction influences treatment decisions, reduces complications, and improves patient outcomes in pleural diseases.
Summary and Clinical Relevance
Transudates are typically caused by systemic factors such as heart failure, liver cirrhosis, or nephrotic syndrome, resulting in low-protein, low-cell pleural fluid due to pressure imbalances. Effusions, often exudates, arise from local inflammation or infection like pneumonia, malignancy, or tuberculosis, characterized by high protein concentration and increased cellularity. Differentiating transudate from exudate using Light's criteria is critical for guiding diagnosis, treatment decisions, and determining the underlying etiology of pleural fluid accumulation.
Transudate Infographic
 libterm.com
libterm.com